Medical Comanagement of Hip Fracture Patients Is Not Associated with Superior Perioperative Outcomes: A Propensity Score-Matched Retrospective Cohort Analysis of the National Surgical Quality Improvement Project
BACKGROUND: Medical comanagement entails a significant commitment of clinical resources with the aim of improving perioperative outcomes for patients admitted with hip fractures. To our knowledge, no national analyses have demonstrated whether patients benefit from this practice.
METHODS: We performed a retrospective cohort analysis of the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) targeted user file for hip fracture 2016-2017. Medical comanagement is a dedicated variable in the NSQIP. Propensity score matching was performed to control for baseline differences associated with comanagement. Matched pairs binary logistic regression was then performed to determine the effect of comanagement on the following primary outcomes: mortality and a composite endpoint of major morbidity.
RESULTS: Unadjusted analyses demonstrated that patients receiving medical comanagement were older and sicker with a greater burden of comorbidities. Comanagement did not have a higher proportion of patients participating in a standardized hip fracture program (53.6% vs 53.7%; P > .05). Comanagement was associated with a higher unadjusted rate of mortality (6.9% vs 4.0%, odds ratio [OR] 1.79: 1.44-2.22; P < .0001) and morbidity (19.5% vs 9.6%, OR 2.28: 1.98-2.63; P < .0001). After propensity score matching was used to control for baseline differences associated with comanagement, patients in the comanagement cohort continued to demonstrate inferior mortality (OR 1.36: 1.02-1.81; P = .033) and morbidity (OR 1.82: 1.52-2.20; P < .0001).
CONCLUSIONS: This analysis does not provide evidence that dedicated medical comanagement of hip fracture patients is associated with superior perioperative outcomes. Further efforts may be needed to refine opportunities to modify the significant morbidity and mortality that persists in this population.
© 2019 Society of Hospital Medicine
METHODS
This study was exempt from the Institutional Review Board review because it uses deidentified data.
We used the targeted hip fracture NSQIP PUF for 2016-2017 to examine perioperative outcomes among patients undergoing hip fracture repair and assess the relationship with medical comanagement, which is a dedicated variable in the NSQIP hip fracture database. We included patients in the comanagement cohort if they received comanagement for part or all of their hip fracture hospitalization.
Demographic, comorbidity, and preoperative variables were examined between the two cohorts. Hypoalbuminemia, as a marker of malnutrition and frailty, was defined as a preoperative serum albumin level <3.5 g/dL, which has demonstrated independent predictive value for adverse outcomes in hip fracture patients in the NSQIP.15,16 Predicted morbidity and mortality rates are calculated as probabilities available for each patient in the PUF based on a NSQIP hierarchical regression analysis of patient-level factors to predict outcomes (eg, not including hospital or provider factors). We also examined the relationship in regard to participation in a standardized hip fracture program (SHFP), which is a multidisciplinary protocolized pathway for hip fracture patients that may include order sets, structured care coordination, involvement of multidisciplinary therapy personnel, and daily milestones and discharge criteria. Participation in an SHFP is recorded in the NSQIP and has demonstrated an association with significantly improved outcomes in this same dataset, the targeted hip fracture PUF.17
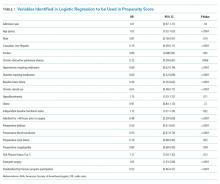
Logistic regression was performed using all baseline variables identified to be significantly different between the cohorts, as well as the following variables with a priori potential importance in predicting membership in the comanagement cohort: admission year, sex, American Society of Anesthesiologists (ASA) physical status ≥4, and participation in an SHFP. Propensity scores were calculated using the significant variables from this model (Table 1) and the abovementioned a priori potential confounders, and then propensity score matching was performed using a greedy matching algorithm (matching ratio 1:1, caliper width = 0.1 pooled standard deviations of the logit of the propensity score) to create comanagement and control cohorts for matched analysis.
The primary outcomes were 30-day mortality and a composite endpoint of major morbidity, including readmission, pulmonary complications (pneumonia, reintubation, prolonged mechanical ventilation, and pulmonary embolism [PE]), septic shock, stroke, myocardial infarction, cardiac arrest, or death. Secondary outcomes included postoperative length of stay, disposition at postoperative day 30, and process compliance measures (proportion of patients allowed to be weight-bearing as tolerated on postoperative day 1, and proportion of patients appropriately prescribed deep venous thrombosis [DVT] prophylaxis for 28 days, proportion of patients appropriately prescribed bone protective medication [eg, vitamin D, bisphosphonates, teriparatide, denosumab, and raloxifene] postoperatively).
Descriptive variables are reported as median (interquartile range) and number (percentage), unless otherwise noted. Continuous outcomes were compared using a Mann–Whitney–Wilcoxon test. Binary outcomes were compared using Fisher’s exact tests (or a Pearson’s Chi-square for more than two response levels) and odds ratios with 95% confidence intervals.