Leveraging the Outpatient Pharmacy to Reduce Medication Waste in Pediatric Asthma Hospitalizations
BACKGROUND AND OBJECTIVE: Previous local quality improvement focused on discharging patients with inhaled corticosteroids (ICS) “in-hand” decreased healthcare reutilization after hospitalization for an asthma exacerbation. However, as a result of these new processes, some patients admitted for an asthma exacerbation received more than one ICS inhaler during their admission, contributing to medication waste and potential patient confusion regarding their discharge medication regimen. We sought to decrease this waste.
METHODS: We conducted a quality improvement project to reduce the prescribing of multiple ICS inhalers to patients at a large academic children’s hospital. Our primary outcome measure was the monthly percentage of patients admitted with an asthma exacerbation who were administered more than one ICS inhaler. A secondary outcome measure evaluated the reliability of the new process of using the hospital-based outpatient pharmacy to supply ICS “in-hand” and verify insurance coverage. After the process map review, we hypothesized a delay in the initial ICS treatment decision would allow for both a finalized discharge medication plan and a standardized process to verify outpatient insurance coverage. |
RESULTS: The mean percentage of patients receiving more than one ICS inhaler decreased from our baseline of 7.4% to 0.7%. Verification of outpatient prescription insurance coverage via the outpatient pharmacy increased from 0.7% to 50%. The average inpatient cost (average wholesale price) for ICS decreased by 62% to $90.25.
CONCLUSIONS: Our process change to use the outpatient pharmacy to dispense and verify insurance coverage for ICS medication was associated with a reduction in medication waste during admission for an asthma exacerbation.
© 2020 Society of Hospital Medicine
METHODS
Context
CCHMC is a quaternary care pediatric health system with more than 600 inpatient beds and 800-900 inpatient admissions per year for acute asthma exacerbation. The Hospital Medicine service cares for patients with asthma on five clinical teams across two different campuses. Care teams are supervised by an attending physician and may include residents, fellows, or nurse practitioners. Patients hospitalized for an acute asthma exacerbation may receive a consult from the Asthma Center consult team, staffed by faculty from either the Pediatric Pulmonology or Allergy/Immunology divisions. Respiratory therapists (RTs) administer inhaled medications and provide asthma education.
Planning the Intervention
Our improvement team included physicians from Hospital Medicine and Pulmonary Medicine, an Asthma Education Coordinator, a Clinical Pharmacist, a Pediatric Chief Resident, and a clinical research coordinator. Initial interventions targeted a single resident team at the main campus before spreading improvement activities to all resident teams at the main campus and then the satellite campus by February 2017.
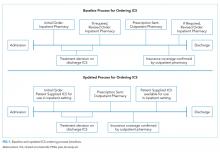
Development of our process map (Figure 1) revealed that the decision for ordering inpatient ICS treatment frequently occurred at admission. Subsequently, the care team or consulting team might make a change in the ICS to fine-tune the outpatient medication regimen given that admission for asthma often results from suboptimal chronic symptom control. Baseline analysis of changes in ICS orders revealed that 81% of ICS changes were associated with a step-up in therapy, defined as an increase in the daily dose of the ICS or the addition of a long-acting beta-agonist. The other common ICS adjustment, accounting for 17%, was a change in corticosteroid without a step-up in therapy, (ie, beclomethasone to fluticasone) that typically occurred near the end of the hospitalization to accommodate outpatient insurance formularies, independent of patient factors related to illness severity.
We utilized the model for improvement and sought to decrease the number of patients administered more than one ICS during an admission through a step-wise quality improvement approach, utilizing plan-do-study-act (PDSA) cycles.10 This study was reviewed and designated as not human subjects research by the CCHMC institutional review board.
Improvement Activities
We conceived key drivers or domains that would be necessary to address to effect change. Key drivers included a standardized process for delayed initiation of ICS and confirmation of outpatient insurance prescription drug coverage, prescriber education, and real-time failure notification.
PDSA Interventions
PDSA 1 & 2: Standardized Process for Initiation of ICS
Our initial tests of change targeted the timing of when an ICS was ordered during hospitalization for an asthma exacerbation. Providers were instructed to delay ordering an ICS until the patient’s albuterol treatments were spaced to every three hours and to include a standardized communication prompt within the albuterol order. The prompt instructed the RT to contact the provider once the patient’s albuterol treatments were spaced to every three hours and ask for an ICS order, if appropriate. This intervention was abandoned because it did not reliably occur.
The subsequent intervention delayed the start of ICS treatment by using a PRN indication advising that the ICS was to be administered once the patient’s albuterol treatments were spaced to every three hours. However, after an error resulted in the PRN indication being included on a discharge prescription for an ICS, the PRN indication was abandoned. Subsequent work to develop a standardized process for delayed initiation of ICS occurred as part of the workflow to address the confirmation of outpatient formulary coverage as described next.