Discharge Medical Complexity, Change in Medical Complexity and Pediatric 30-day Readmission
BACKGROUND: While medical complexity is associated with pediatric readmission risk, less is known about how increases in medical complexity during hospitalization affect readmission risk.
METHODS: We conducted a five-year retrospective, case-control study of pediatric hospitalizations at a tertiary care children’s hospital. Cases with a 30-day unplanned readmission were matched to controls based on admission seasonality and distance from the hospital. Complexity variables included the number of medications prescribed at discharge, medical technology, and the need for home healthcare services. Change in medical complexity variables included new complex chronic conditions and new medical technology. We estimated odds of 30-day unplanned readmission using adjusted conditional logistic regression.
RESULTS: Of 41,422 eligible index hospitalizations, we included 595 case and 595 control hospitalizations. Complexity: Polypharmacy after discharge was common. In adjusted analyses, being discharged with ≥2 medications was associated with higher odds of readmission compared with being discharged without medication; children with ≥5 discharge medications had a greater than four-fold higher odds of readmission. Children assisted by technology had higher odds of readmission compared with children without technology assistance. Change in complexity: New diagnosis of a complex chronic condition (Adjusted Odds Ratio (AOR) = 1.75; 1.11-2.75) and new technology (AOR = 1.84; 1.09-3.10) were associated with higher risk of readmission when adjusting for patient characteristics. However, these associations were not statistically significant when adjusting for length of stay.
CONCLUSION: Polypharmacy and use of technology at discharge pose a substantial readmission risk for children. However, added technology and new complex chronic conditions do not increase risk when accounting for length of stay.
© 2019 Society of Hospital Medicine
RESULTS
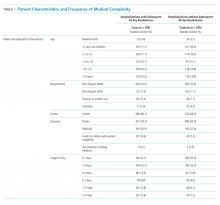
Of the 41,422 eligible index hospitalizations during the study period, 9.4% resulted in a 30-day unplanned readmission. After randomly selecting one hospitalization per child, there were 781 eligible cases. We subsequent matched all but one eligible case to a control. We randomly selected encounters for medical record review, reviewing a total of 1,212 encounters. After excluding pairs with incomplete records, we included 595 cases and 595 controls in this analysis (Figure). Patient/hospitalization characteristics are displayed in Table 1. The most frequent primary discharge diagnoses are displayed in Appendix Table 1.
Models of Medical Complexity at Discharge
Polypharmacy after discharge was common for both readmitted and nonreadmitted patients. Children who experienced unplanned readmission in 30 days were discharged with a median of four different scheduled medications (interquartile range [IQR] 2,7) which translated into a median of six (IQR 3,12) scheduled doses in a 24-hour period. In comparison, children without an unplanned readmission had a median of two different scheduled medications (IQR 1,3) with a median of three (IQR 0,7) scheduled doses in a 24-hour period. Medical technology was more common in case children (42%) than in control children (14%). Central lines and enteral tubes were the most common forms of medical technology in both cases and controls. Home health referral was common in both cases (44%) and controls (23%; Table 1).
In Model 1 (adjusting only for patient characteristics; Table 3), being discharged on two or more scheduled medications was associated with higher odds of readmission compared to being discharged without medications, with additional medications associated with even higher odds of readmission. Children with any technology had higher odds of readmission than children without medical technology. Likewise, home healthcare visits after discharge were associated with elevated odds of readmission in multivariable analyses without LOS. However, after adding LOS to the model (Model 2), home healthcare visits were no longer significantly associated with readmission.
Change in Medical Complexity Models
The adjudication of new CCCs had good reliability (Κ = 0.72). New CCCs occurred in 18% and new technologies occurred in 17% of cases. Comparatively, new CCCs occurred in 10% and new technologies in 7% of hospitalizations in control children (Table 1). In bivariate analyses, both aspects of change in medical complexity were associated with higher odds of readmission (Table 2). In multivariate analysis with patient characteristics (Model 3; Table 3), all aspects of change in complexity were associated with elevated odds of readmission. A new CCC was associated with higher odds of readmission (adjusted OR (AOR) 1.75, 95% CI: 1.11-2.75) as was new technology during admission (AOR 1.84, 95%CI: 1.09-3.10). Furthermore, the odds of readmission for medical complexity variables (polypharmacy and home healthcare need) remained largely unchanged when adding the change in medical complexity variables (ie, comparing Model 1 and Model 3). However, when accounting for LOS (Model 4), neither the acquisition of a new CCC nor the addition of new technology was associated with readmission. The most common form of new technology was central line followed by nonsurgically placed enteral tube (Appendix Table 2). Finally, in sensitivity analyses (results not detailed), separating new CCC acquired at birth and new CCCs in nonbirth hospitalizations, compared to hospitalizations with no new CCC, yielded similar results as the primary analyses.