Collaboration, Not Calculation: A Qualitative Study of How Hospital Executives Value Hospital Medicine Groups
BACKGROUND: Hospital medicine groups (HMGs) typically receive financial support from hospitals. Determining a fair amount of financial support requires negotiation between HMG and hospital leaders. As the hospital medicine care model evolves, hospital leaders may regularly challenge HMGs to demonstrate the financial value of activities that do not directly generate revenue.
OBJECTIVE: To describe current attitudes and beliefs of hospital executives regarding the value of contributions made by HMGs. DESIGN: Thematic content analysis of key informant interviews.
PARTICIPANTS: Twenty-four healthcare institutional leaders, including hospital presidents, chief medical officers, chief executive officers, and chief financial officers. Participants comprised a diverse sample from all regions in the United States, including rural, suburban, and urban locations, and academic and nonacademic institutions.
RESULTS: Executives highly valued hospitalist groups that demonstrate alignment with hospital priorities, and often used this concept to summarize the HMG’s success across several value domains. Most executives evaluated only a few key HMG metrics, but almost no executives reported calculating the HMG return on investment by summing pertinent quantitative contributions. Respondents described an evolving concept of hospitalist value and believed that HMGs generate substantial value that is difficult to measure financially.
CONCLUSIONS: Hospital executives appear to make financial support decisions based on a small number of basic financial or care quality metrics combined with a subjective assessment of the HMG’s broader alignment with hospital priorities. HMG leaders should focus on building relationships that facilitate dialog about alignment with hospital needs.
© 2019 Society of Hospital Medicine
Interview Guide and Data Collection
All interviews followed a guide with eight demographic questions and 10 open-ended questions (Appendix). Cognitive interviews were performed with two hospital executives outside the study cohort, resulting in the addition of one question and rewording one question for clarity. One-on-one interviews were performed by 10 committee members (range, 1-3 interviews). All interview audios were recorded, and no field notes were kept. The goal of the interviews was to obtain an understanding of how hospital executives value the contributions and costs of hospitalist groups.
The interviews began with questions about the informant’s current interactions with hospitalists and the origin of the hospitalist group at their facility. Informants then described the value they feel hospitalists bring to their hospital and occasions they were surprised or dissatisfied with the clinical or financial value delivered by the hospitalists. Participants described how they calculate a return on investment (ROI) for their hospitalist group, nonfinancial benefits and disadvantages to hospitalists, and how they believe hospitalists should participate in risk-sharing contracts.
Data Analysis
The interview audiotapes were transcribed and deidentified. A sample of eight transcripts was verified by participants to ensure accuracy. Three investigators (AAW, RC, CC) reviewed a random sample of five transcripts to identify and codify preliminary themes. We applied a general inductive framework with a content analysis approach. Two investigators (TM and MC) read all transcripts independently, coding the presence of each theme and quotations exemplifying these themes using qualitative analysis software (Dedoose Version 7.0.23, SocioCultural Research Consultants). A third investigator (AAW) read all the transcripts and resolved differences of opinion. Themes and code application were discussed among the study team after the second and fifth transcripts to add or clarify codes. No new codes were identified after the first review of the preliminary codebook, although investigators intermittently used an “unknown” code through the 20th transcript. After discussion to reach consensus, excerpts initially coded “unknown” were assigned existing codes; the 20th transcript represents the approximate point of reaching thematic saturation.
RESULTS
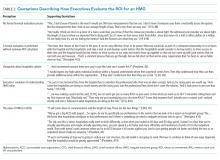
Of the 24 participants, 18 (75%) were male, representing a variety of roles: 7 (29.2%) CMOs, 5 (20.8%) Presidents, 5 (20.8%) CFOs, 4 (16.7%) CEOs, and 3 (12.5%) Vice Presidents. The participants represented all regions (Midwest 12 [50%], South 6 [25%], West 4 [16.7%], and East 2 [8.3%], community size (Urban 11 [45.8%], Suburban 8 [33.3%], and Rural 5 [20.8%]), and Hospital Types (Community 11 [45.8%], Multihospital System 5 [20.8%], Academic 5 [20.8%], Safety Net 2 [8.3%], and Critical Access 1 [4.2%]). We present specific themes below and supporting quotations in Tables 1 and 2.
Current Value of the HMG at the Respondent’s Hospital
Most executives reported their hospital’s HMG had operated for over a decade and had developed an earlier, outdated value framework. Interviewees described an initial mix of financial pressures, shifts in physician work preferences, increasing patient acuity, resident labor shortages, and unsolved hospital throughput needs that triggered a reactive conversion from community PCP staffing to hospitalist care teams, followed by refinements to realize value.