Assess Before Rx: Reducing the Overtreatment of Asymptomatic Blood Pressure Elevation in the Inpatient Setting
BACKGROUND: Asymptomatic blood pressure elevation is common in the inpatient setting. National guidelines recommend treating with oral agents to slowly decrease blood pressure; however, many clinicians use intravenous antihypertensive medications, which can lead to unpredictable changes in blood pressure.
OBJECTIVE: To decrease the number of inappropriate orders (without symptoms of hypertensive emergency or order for NPO) of intravenous antihypertensives and adverse events associated with intravenous orders.
DESIGN: Quasi-experimental study with multidisciplinary intervention. PARTICIPANTS: Inpatients with a one-time order for an intravenous antihypertensive agent from January 2016 to February 2018.
MAIN MEASURES: The main outcomes were the total numbers of orders and inappropriate orders, adverse events, and alternate etiologies per 1,000 patient-days. As a balancing measure, patients were monitored for adverse events when blood pressure was elevated and not treated.
KEY RESULTS: There were a total of 260 one-time orders of intravenous antihypertensives on two medical units. Inappropriate orders decreased from 8.3 to 3.3 per 1,000 patient days (P = .0099). Adverse events associated with intravenous antihypertensives decreased from 3.7 to 0.8 per 1,000 patient days (P = .0072).
CONCLUSION: This initiative demonstrated a significant reduction in inappropriate use of IV antihypertensives and an associated reduction in adverse events.
© 2019 Society of Hospital Medicine
Treatment Algorithm and Education
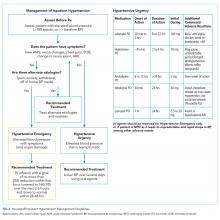
A clinical algorithm was designed with nursing and cardiology representatives to provide guidance for nurses regarding the best practice for evaluation of inpatient hypertension, focusing on assessing patients before recommending treatment (“Assess Before Rx”; Figure 1). Educational sessions reinforcing the clinical algorithm were held monthly at nursing huddles. These involved an introduction session providing the background and purpose of the project, with follow-up sessions including interactive mock cases on the assessment of hypertensive urgency.
A second treatment algorithm was designed, with housestaff and cardiology input, to provide guidance for the internal medicine housestaff and nurse practitioners. It utilized a similar approach regarding identification, evaluation, and assessment of alternate etiologies but included more detailed treatment recommendations with a table outlining the oral medications used for hypertensive urgency (Figure 2). The flowchart and table were uploaded to an existing mobile application used by housestaff and nurse practitioners for quick access. The mobile application is frequently used by housestaff and contains many clinical resources. Additionally, e-mails including the purpose of the project and the treatment algorithm were sent to rotating housestaff at the start of each new medicine rotation.
Audit and Feedback
Monthly feedback was e-mailed to the nurses, which reinforced the goals and provided positive feedback on outcomes with an announcement of the “Nurse of the Month.” The winners were selected based on the most accurate and appropriate documentation of their assessments determined through retrospective chart review.
Targeted e-mail feedback was also sent to providers who ordered IV antihypertensives without the appropriate indication. The e-mails included the medical record number, date and time of the order, any alternate etiologies that were documented, and any adverse events that occurred as a result of the medication.
Systems Change: Electronic Medical Record Orders
EMR advisory warnings were placed on IV antihypertensive orders of labetalol and hydralazine. The alerts served to nonintrusively remind providers to assess for symptoms before placing the order to ensure that the order was appropriate.
Data Collection and Assessment
Seven-month preintervention (January-July 2016) and 12-month postintervention (March 2017-February 2018) data were compared. The months prior to intervention were excluded to account for project development and educational lag. Data were obtained from EMR utilization reports of one-time orders of IV labetalol and hydralazine, and retrospective chart review. Patients who were pregnant, less than 18 years of age, or postoperative were excluded. Orders were designated as inappropriate if there was no evidence of hypertensive emergency through documentation in progress notes, or if the patient was able to take oral medication (not NPO). Adverse events were defined as a blood pressure drop of more than 25%, a change in the heart rate by more than 20 beats per minute, or the need for IV fluids, based on previous studies.7 Although decreased blood pressure is not necessarily dangerous in and of itself, adverse events arising from blood pressure decreasing too rapidly from IV antihypertensives are well documented.9,11 The presence of alternate etiologies of high blood pressure that were documented in progress notes, including pain, anxiety, agitation, and holding of home blood pressure medications, were recorded. The numbers of inappropriate orders pre- and postintervention were compared. Confounding factors of patient age and length of stay (LOS) were compared pre- and postintervention in order to rule out other factors to which the intervention’s effect could be attributed.