Patient, Caregiver, and Clinician Perspectives on Expectations for Home Healthcare after Discharge: A Qualitative Case Study
BACKGROUND: Patients discharged from the hospital with skilled home healthcare (HHC) services have multiple comorbidities, high readmission rates, and multiple care needs. In prior work, HHC nurses described that patients often express expectations for services beyond the scope of skilled HHC.
OBJECTIVE: The objective of this study is to evaluate and compare expectations for HHC from the patient, caregiver, and HHC perspectives after hospital discharge.
DESIGN/PARTICIPANTS: This was a descriptive qualitative case study including HHC patients, caregivers, and clinicians. Patients were discharged from an academic medical center between July 2017 and February 2018.
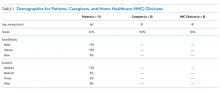
RESULTS: The sample (N = 27) included 11 HHC patients, eight caregivers, and eight HHC clinicians (five nurses and three physical therapists). Patient mean age was 66 years and the majority were female, white, and had Medicare. We observed main themes of clear and unclear expectations for HHC after discharge. Clear expectations occur when the patient and/or caregiver have expectations for HHC aligned with the services received. Unclear expectations occur when the patient and/or caregiver expectations are uncertain or misaligned with the services received. Patients and caregivers with clear expectations for HHC frequently described prior experiences with skilled HHC or work experience within the healthcare field. In most cases with unclear expectations, the patient and caregiver did not have prior experience with HHC.
CONCLUSIONS: To improve HHC transitions, we recommend actively engaging both patients and caregivers in the hospital and HHC settings to provide education about HHC services, and assess and address additional care needs.
© 2019 Society of Hospital Medicine
Patient interviews lasted an average of 43 minutes, caregiver interviews an average of 41 minutes, and HHC clinician interviews an average of 25 minutes
We observed the two main themes of clear and unclear expectations for HHC after discharge. Clear expectations occur when the patient and/or caregiver have expectations for HHC that align with the services they receive. Unclear expectations occur when the patient and/or caregiver expectations are either uncertain or misaligned with the services they receive. Although not all interviews yielded codes about clear or unclear expectations, patients described clear expectations in five cases and unclear expectations in another five cases.
In nine cases with more than one perspective available, expectations were compared within cases and found to be clear (three cases), unclear (three cases), or discordant (three cases) across perspectives. For the discordant cases, the description of clear and unclear expectations differed between patients and either their caregiver or their HHC clinician. Patients and caregivers with clear expectations for HHC frequently described prior experiences with skilled HHC or work experience within the healthcare field. In most cases with unclear expectations, the patient and caregiver did not have prior experience with HHC. In addition, the desire for assistance with personal care for patients such as showering and housekeeping was described by caregivers with unclear expectations. The results are organized into clear, unclear, and discordant expectations from the perspectives of patients, caregivers, and HHC clinicians within cases.