Impact of a Multicenter, Mentored Quality Collaborative on Hospital-Associated Venous Thromboembolism
BACKGROUND: Reliable prophylaxis of hospital-associated venous thromboembolism (HA-VTE) is not achieved in many hospitals. Efforts to improve prophylaxis have had uneven results.
OBJECTIVE: To reduce HA-VTE with a scalable quality improvement collaborative.
DESIGN: A prospective, unblinded, open-intervention study with historical controls.
PARTICIPANTS AND SETTING: All adult inpatients at 35 community hospitals in California, Arizona, and Nevada.
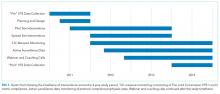
INTERVENTIONS: A centrally supported collaborative implementing standardized VTE risk assessment and prophylaxis. Protocols were developed with 9 “pilot” sites, which received individualized mentoring. Finished protocols were disseminated to 26 “spread” sites, which received improvement webinars without mentoring. Active surveillance for real-time correction of suboptimal prophylaxis was funded in pilot sites and encouraged in spread sites. Planning and minimal improvement work began in 2011; most implementation occurred in 2012 and 2013.
MEASUREMENTS: Rates of per-protocol prophylaxis (at pilot sites), and compliance with The Joint Commission VTE measures (all sites), were monitored starting in January 2012. The International Classification of Diseases, 9th Edition-Clinical Modification codes were used to determine the rates of HA-VTE within 30 days of discharge, heparin-induced thrombocytopenia, and anticoagulation adverse events; preimplementation (2011) rates were compared with postimplementation (2014) rates.
RESULTS: Protocol-appropriate prophylaxis rates and The Joint Commission measure compliance both reached 97% in 2014, up from 70% to 89% in 2012 and 2013. Five thousand three hundred and seventy HA-VTEs occurred during 1.16 million admissions. Four hundred twenty-eight fewer HA-VTEs occurred in 2014 than in 2011 (relative risk 0.78; 95% confidence interval, 0.73-0.85). HA-VTEs fell more in pilot sites than spread sites (26% vs 20%). The rates of adverse events were reduced or unchanged.
CONCLUSIONS: Collaborative efforts were associated with improved prophylaxis rates and fewer HA-VTEs.
© 2018 Society of Hospital Medicine
Multidisciplinary Teams
Improvement teams formed between March 2011 and September 2012. Members included a physician champion, frontline nurses and physicians, an administrative liaison, pharmacists, quality and data specialists, clinical informatics staff, and stakeholders from key clinical services. Teams met at least monthly at each site.
Physician Mentors
The 9 pilot sites received individualized mentorship provided by outside experts (IJ or GM) based on a model pioneered by the Society of Hospital Medicine’s (SHM) Mentored Implementation programs.23 Each pilot site completed a self-assessment survey17 (see supplementary Appendix A) about past efforts, team composition, current performance, aims, barriers, and opportunities. The mentors reviewed the completed questionnaire with each hospital and provided advice on the VTE protocol and order set design, measurement, and benchmarking during 3 webinar meetings scheduled at 0, 3, and 9 months, plus as-needed e-mail and phone correspondence. After each webinar, the mentors provided detailed improvement suggestions (see supplementary Appendix B). Several hospitals received mentor site visits, which focused on unit rounding, active surveillance, staff and provider education, and problem-solving sessions with senior leadership, physician leadership, and the improvement team.
VTE Protocol
After a literature review and consultation with the mentors, Dignity Health developed and implemented a VTE protocol, modified from a model used in previous improvement efforts.18,22-24 Its risk assessment method is often referred to as a “3 bucket” model because it assigns patients to high-, moderate-, or low-risk categories based on clinical factors (eg, major orthopedic surgery, prior VTE, and others), and the VTE protocol recommends interventions based on the risk category (see supplementary Appendix C). Dignity Health was transitioning to a single electronic health record (Cerner Corporation, North Kansas City, MO) during the study, and study hospitals were using multiple platforms, necessitating the development of both paper and electronic versions of the VTE protocol. The electronic version required completion of the VTE protocol for all inpatient admissions and transfers. The VTE protocol was completed in November 2011 and disseminated to other sites in a staggered fashion through November 2012. Completed protocols and improvement tips were shared by the project lead and by webinar sessions. Sites were also encouraged to implement a standardized practice that allowed nurses to apply sequential compression devices to at-risk patients without physician orders when indicated by protocol, when contraindications such as vascular disease or ulceration were absent.
Education
Staff were educated about the VTE protocol by local teams, starting between late 2011 and September 2012. The audience (physicians, nurses, pharmacists, etc.) and methods (conferences, fliers, etc.) were determined by local teams, following guidance by mentors and webinar content. Active surveillance provided opportunities for in-the-moment, patient-specific education and protocol reinforcement. Both mentors delivered educational presentations at pilot sites.
Active Surveillance
Sites were encouraged to perform daily review of prophylaxis adequacy for inpatients and correct lapses in real time (both under- and overprophylaxis). Inappropriate prophylaxis orders were addressed by contacting providers to change the order or document the rationale not to. Lapses in adherence to prophylaxis were addressed by nursing correction and education of involved staff. Active surveillance was funded for 10 hours a week at pilot sites. Spread sites received only minimal support from HEN monies. All sites used daily prophylaxis reports, enhanced to include contraindications like thrombocytopenia and coagulopathy, to facilitate efforts. Active surveillance began in May 2012 in the lead pilot hospitals and was implemented in other sites between October 2012 and February 2013.
Metrics
Prophylaxis Rates
Measurement of prophylaxis did not begin until 2012 to 2013; thus, the true baseline rate for prophylaxis was not captured. TJC metrics (VTE-1 and VTE-2)25 were consolidated into a composite TJC prophylaxis rate from January 2012 to December 2014 for both pilot and spread hospitals. These measures assess the percentage of adult inpatients who received VTE prophylaxis or have documentation of why no prophylaxis was given the day of or day after hospital admission (VTE-1) or the day of or day after ICU admission or transfer (VTE-2). These measures are met if any mechanical or pharmacologic prophylaxis was delivered.
In addition to the TJC metric, the 9 pilot hospitals monitored rates of protocol-compliant prophylaxis for 12 to 20 months. Each patient’s prophylaxis was considered protocol compliant if it was consistent with the prophylaxis protocol at the time of the audit or if contraindications were documented (eg, patients eligible for, but with contraindications to, pharmacologic prophylaxis had to have an order for mechanical prophylaxis or documented contraindication to both modalities). As this measure was initiated in a staggered fashion, the rate of protocol-compliant prophylaxis is summarized for consecutive months of measurement rather than consecutive calendar months.