Issues Identified by Postdischarge Contact after Pediatric Hospitalization: A Multisite Study
BACKGROUND: Many hospitals are considering contacting hospitalized patients soon after discharge to help with issues that arise.
OBJECTIVES: To (1) describe the prevalence of contact-identified postdischarge issues (PDI) and (2) assess characteristics of children with the highest likelihood of having a PDI.
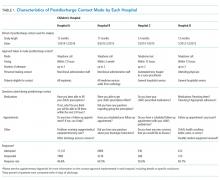
DESIGN, SETTING, AND PATIENTS: A retrospective analysis of hospital-initiated follow-up contact for 12,986 children discharged from January 2012 to July 2015 from 4 US children’s hospitals. Contact was made within 14 days of discharge by hospital staff via telephone call, text message, or e-mail. Standardized questions were asked about issues with medications, appointments, and other PDIs. For each hospital, patient characteristics were compared with the likelihood of PDI by using logistic regression.
RESULTS: Median (interquartile range) age of children at admission was 4.0 years (0-11); 59.9% were non-Hispanic white, and 51.0% used Medicaid. The most common reasons for admission were bronchiolitis (6.3%), pneumonia (6.2%), asthma (5.1%), and seizure (4.9%). Twenty-five percent of hospitalized children (n = 3263) reported a PDI at contact (hospital range: 16.0%-62.8%). Most (76.3%) PDIs were related to follow-up appointments (eg, difficulty getting one); 20.8% of PDIs were related to medications (eg, problems filling a prescription). Patient characteristics associated with the likelihood of PDI varied across hospitals. Older age (age 10-18 years vs <1 year) was significantly (P < .001) associated with an increased likelihood of PDI in 3 of 4 hospitals.
CONCLUSIONS: PDIs were identified often through hospital-initiated follow-up contact. Most PDIs were related to appointments. Hospitals caring for children may find this information useful as they strive to optimize their processes for follow-up contact after discharge.
© 2018 Society of Hospital Medicine
Many hospitals are considering or currently employing initiatives to contact patients after discharge. Whether conducted via telephone or other means, the purpose of the contact is to help patients adhere to discharge plans, fulfill discharge needs, and alleviate postdischarge issues (PDIs). The effectiveness of hospital-initiated postdischarge phone calls has been studied in adult patients after hospitalization, and though some studies report positive outcomes,1-3 a 2006 Cochrane review found insufficient evidence to recommend for or against the practice.4
Little is known about follow-up contact after hospitalization for children.5-11 Rates of PDI vary substantially across hospitals. For example, one single-center study of postdischarge telephone contact after hospitalization on a general pediatric ward identified PDIs in ~20% of patients.10 Another study identified PDIs in 84% of patients discharged from a pediatric rehabilitation facility.11 Telephone follow-up has been associated with reduced health resource utilization and improved patient satisfaction for children discharged after an elective surgical procedure6 and for children discharged home from the emergency department.7-9
More information is needed on the clinical experiences of postdischarge contact in hospitalized children to improve the understanding of how the contact is made, who makes it, and which patients are most likely to report a PDI. These experiences are crucial to understand given the expense and time commitment involved in postdischarge contact, as many hospitals may not be positioned to contact all discharged patients. Therefore, we conducted a pragmatic, retrospective, naturalistic study of differing approaches to postdischarge contact occurring in multiple hospitals. Our main objective was to describe the prevalence and types of PDIs identified by the different approaches for follow-up contact across 4 children’s hospitals. We also assessed the characteristics of children who have the highest likelihood of having a PDI identified from the contact within each hospital.
METHODS
Study Design, Setting, and Population
Main Outcome Measures
The main outcome measure was identification of a PDI, defined as a medication, appointment, or other discharge-related issue, that was reported and recorded by the child’s caregiver during conversation from the standardized questions that were asked during follow-up contact as part of routine discharge care (Table 1). Medication PDIs included issues filling prescriptions and tolerating medications. Appointment PDIs included not having a follow-up appointment scheduled. Other PDIs included issues with the child’s health condition, discharge instructions, or any other concerns. All PDIs had been recorded prospectively by hospital contact personnel (hospitals A, B, and D) or through an automated texting system into a database (hospital C). Where available, free text comments that were recorded by contact personnel were reviewed by one of the authors (KB) and categorized via an existing framework of PDI designed by Heath et al.10 in order to further understand the problems that were reported.
Patient Characteristics
Patient hospitalization, demographic, and clinical characteristics were obtained from administrative health data at each institution and compared between children with versus without a PDI. Hospitalization characteristics included length of stay, season of admission, and reason for admission. Reason for admission was categorized by using 3M Health’s All Patient Refined Diagnosis Related Groups (APR-DRG) (3M, Maplewood, MN). Demographic characteristics included age at admission in years, insurance type (eg, public, private, and other), and race/ethnicity (Asian/Pacific Islander, Hispanic, non-Hispanic black, non-Hispanic white, and other).