A Contemporary Assessment of Mechanical Complication Rates and Trainee Perceptions of Central Venous Catheter Insertion
BACKGROUND: Limited data exist regarding rates of mechanical complications of ultrasound-guided, nontunneled central venous catheters (CVC). Similarly, trainee perceptions surrounding CVC complications are largely unknown.
OBJECTIVES: To evaluate contemporary CVC mechanical complication rates, associated risk factors, and trainee perspectives.
DESIGN: A single-center retrospective review of CVC procedures between June 1, 2014, and May 1, 2015. Electronic survey distributed to internal medicine trainees.
SETTING: Intensive care units and the emergency department at an academic hospital.
MEASUREMENTS: Electronic health records of patients with CVC procedures were reviewed for complications. Demographic and procedural characteristics were compared for complicated vs uncomplicated procedures. Student t tests and chi-square tests were used to compare continuous and categorical variables, respectively.
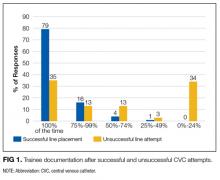
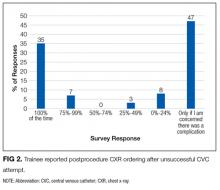
RESULTS: Of the 730 reviewed records, 14 serious mechanical complications occurred due to pneumothorax (n = 5), bleeding (n = 3), vascular injury (n = 3), stroke (n = 1), and death (n = 2). Risk factors for complicated vs uncomplicated CVC placement included subclavian location (21.4% vs 7.8%, P = 0.001), number of attempts (2.2 vs 1.5, P = 0.02), unsuccessful CVC (21.4% vs. 4.3%, P = 0.001), attending supervision (61.5% vs 34.7%, P = 0.04), low body mass index (mean 25.7 kg/m2 vs 31.5 kg/m2, P = 0.001), anticoagulation (28.6% vs 20.6%, P = 0.048), and ventilation (78.5% vs 66.5%, P = 0.001). Survey data suggested deficiencies in managing unsuccessful CVC procedures; specifically, only 35% (N = 21/60) of trainees regularly perform chest x-rays after failed CVC attempt.
CONCLUSIONS: We observed a 1.9% rate of mechanical complications associated with CVC placement. Our study confirms historical data that unsuccessful CVC attempts are an important risk factor for complications. Education regarding unsuccessful CVC placement may improve patient safety. Journal of Hospital Medicine 2017;12:646-651. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Risk Factors for Mechanical Complications
Certain patient factors were more commonly associated with complications. For example, BMI was significantly lower in the group that experienced complications vs those that did not (25.7 vs 31.0 kg/m2, P = 0.001). No other associations between demographic factors, including age (61.4 years vs 58.9 years, P = 0.57) or sex (57.1% male vs 41.3% female, P = 0.24), or admission APACHE III score (96 vs 86, P = 0.397) were noted. The mean INR, platelets, and lactate did not differ between the 2 groups. There was no difference between the use of vasopressors. Ventilator use (including endotracheal tube or NIPPV) was found to be significantly higher in the group that experienced mechanical complications (78.5% vs 65.9%, P = 0.001). Anticoagulation use was also associated with mechanical complications (28.6% vs 20.6%, P = 0.05); 3 patients on anticoagulation experienced significant hematomas. Mechanical complications were more common with subclavian location (21.4% vs 7.8%, P = 0.001); in all 3 cases involving subclavian CVC placement, the complication experienced was pneumothorax. The number of attempts significantly differed between the 2 groups, with an average of 1.5 attempts in the group without complications and 2.2 attempts in the group that experienced complications (P = 0.02). Additionally, rates of successful placement were lower among patients who experienced complications (78.6% vs 95.7%, P = 0.001).
With respect to operator characteristics, no significant difference between the levels of training was noted among those who experienced complications vs those who did not. Attending supervision was more frequent for the group that experienced complications (61.5% vs 34.2%, P = 0.04). There was no significant difference in complication rate according to the first vs the second half of the academic year (0.4% vs 0.3% per month, P = 0.30) or CVC placement during the day vs night (1.9% vs 2.0%, P = 0.97). A trend toward more complications in CVCs placed over the weekend compared to a weekday was observed (2.80% vs 1.23%, P = 0.125).
Unsuccessful CVCs
There were 30 documented unsuccessful CVC procedures, representing 4.1% of all procedures. Of these, 3 procedures had complications; these included 2 pneumothoraxes (1 leading to death) and 1 unexplained death. Twenty-four of the unsuccessful CVC attempts were in either the subclavian or IJ location; of these, 5 (21%) did not have a postprocedure CXR obtained.
Survey Results
The survey was completed by 103 out of 166 internal medicine residents (62% response rate). Of these, 55% (n = 57) reported having performed 5 or more CVCs, and 14% (n = 14) had performed more than 15 CVCs.
All respondents who had performed at least 1 CVC (n = 80) were asked about their perceptions regarding attending supervision. Eighty-one percent (n = 65/80) responded that they have never been directly supervised by an attending during CVC placement, while 16% (n = 13/80) reported being supervised less than 25% of the time. Most (n = 53/75, 71%) did not feel that attending supervision affected their performance, while 21% (n = 16/75) felt it affected performance negatively, and only 8% (n = 6/75) stated it affected performance positively. Nineteen percent (n = 15/80) indicated that they prefer more supervision by attendings, while 35% (n = 28/80) did not wish for more attending supervision, and 46% (n = 37/80) were indifferent.
DISCUSSION
We performed a contemporary analysis of CVC placement at an academic tertiary care center and observed a rate of severe mechanical complications of 1.9%. This rate is within previously described acceptable thresholds.16 Our study adds to the literature by identifying several important risk factors for development of mechanical complications. We confirm many risk factors that have been noted historically, such as subclavian line location,2,3 attending supervision,3 low BMI,4 number of CVC attempts, and unsuccessful CVC placement.3,4,7,15 We identified several unique risk factors, including systemic anticoagulation as well as ventilator use. Lastly, we identified unexpected deficits in trainee knowledge surrounding management of failed CVCs and negative attitudes regarding attending supervision.