A Contemporary Assessment of Mechanical Complication Rates and Trainee Perceptions of Central Venous Catheter Insertion
BACKGROUND: Limited data exist regarding rates of mechanical complications of ultrasound-guided, nontunneled central venous catheters (CVC). Similarly, trainee perceptions surrounding CVC complications are largely unknown.
OBJECTIVES: To evaluate contemporary CVC mechanical complication rates, associated risk factors, and trainee perspectives.
DESIGN: A single-center retrospective review of CVC procedures between June 1, 2014, and May 1, 2015. Electronic survey distributed to internal medicine trainees.
SETTING: Intensive care units and the emergency department at an academic hospital.
MEASUREMENTS: Electronic health records of patients with CVC procedures were reviewed for complications. Demographic and procedural characteristics were compared for complicated vs uncomplicated procedures. Student t tests and chi-square tests were used to compare continuous and categorical variables, respectively.
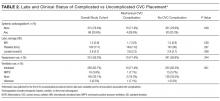
RESULTS: Of the 730 reviewed records, 14 serious mechanical complications occurred due to pneumothorax (n = 5), bleeding (n = 3), vascular injury (n = 3), stroke (n = 1), and death (n = 2). Risk factors for complicated vs uncomplicated CVC placement included subclavian location (21.4% vs 7.8%, P = 0.001), number of attempts (2.2 vs 1.5, P = 0.02), unsuccessful CVC (21.4% vs. 4.3%, P = 0.001), attending supervision (61.5% vs 34.7%, P = 0.04), low body mass index (mean 25.7 kg/m2 vs 31.5 kg/m2, P = 0.001), anticoagulation (28.6% vs 20.6%, P = 0.048), and ventilation (78.5% vs 66.5%, P = 0.001). Survey data suggested deficiencies in managing unsuccessful CVC procedures; specifically, only 35% (N = 21/60) of trainees regularly perform chest x-rays after failed CVC attempt.
CONCLUSIONS: We observed a 1.9% rate of mechanical complications associated with CVC placement. Our study confirms historical data that unsuccessful CVC attempts are an important risk factor for complications. Education regarding unsuccessful CVC placement may improve patient safety. Journal of Hospital Medicine 2017;12:646-651. © 2017 Society of Hospital Medicine
© 2017 Society of Hospital Medicine
Primary Outcome
The primary outcome was the rate of severe mechanical complications related to CVC placement. Similar to prior studies,2 we defined severe mechanical complications as arterial placement of dilator or catheter, hemothorax, pneumothorax, cerebral ischemia, patient death (related to procedure), significant hematoma, or vascular injury (defined as complication requiring expert consultation or blood product transfusion). We did not require a lower limit on blood transfusion. We considered pneumothorax a complication regardless of whether chest tube intervention was performed, as pneumothorax subjects the patient to additional tests (eg, serial CXRs) and sometimes symptoms (shortness of breath, pain, anxiety) regardless of whether or not a chest tube was required. Complications were confirmed by a direct review of procedure notes, progress notes, discharge summaries, and imaging studies.
Trainee Survey
A survey was electronically disseminated to all internal medicine and medicine-pediatric residents to inquire about CVC experiences, including time spent in the medical ICU, number of CVCs performed, postprocedure behavior for both failed and successful CVCs, and supervision experience and attitudes. Please see supplemental materials for full survey contents.
Statistical Methods
Descriptive statistics (percentage) were used to summarize data. Continuous and categorical variables were compared using Student t tests and chi-square tests, respectively. All analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
Ethical and Regulatory Oversight
The study was deemed exempt by the University of Michigan Institutional Review Board (HUM00100549) as data collection was part of a quality improvement effort.
RESULTS
Demographics and Characteristics of Device Insertion
Between June 1, 2014, and May 1, 2015, 730 CVC procedure notes were reviewed (Table 1). The mean age of the study population was 58.9 years, and 41.6% (n = 304) were female. BMI data were available in 400 patients without complications and 5 patients with complications; the average BMI was 31.5 kg/m2. The APACHE III score was available for 442 patients without complications and 10 patients with complications; the average score was 86 (range 19-200). Most of the CVCs placed (n= 504, 69%) were small bore (<7 Fr). The majority of catheters were placed in the internal jugular (IJ) position (n = 525, 71.9%), followed by femoral (n = 144, 19.7%), subclavian (N = 57, 7.8%), and undocumented (n = 4, 0.6%). Ninety-six percent (n = 699) of CVCs were successfully placed. Seventy-six percent (n = 558) of procedure notes included documentation of the number of CVC attempts; of these, 85% documented 2 or fewer attempts. The majority of CVCs were placed by residents (n = 537, 73.9%), followed by fellows (N = 127, 17.5%) and attendings (n = 27, 3.7%). Attending supervision for all or key portions of CVC placement occurred 34.7% (n = 244) of the time overall and was lower for internal medicine trainees (n = 98/463, 21.2%) compared with surgical trainees (n = 73/127, 57.4%) or emergency medicine trainees (n = 62/96, 64.6%; P < 0.001). All successful IJ and subclavian CVCs except for 2 insertions (0.3%) had a postprocedure CXR. A minority of notes documented pressure transduction (4.5%) or blood gas analysis (0.2%) to confirm venous placement.
Mechanical Complications
The mechanical complications identified included pneumothorax (n = 5), bleeding requiring transfusion (n = 3), vascular injury requiring expert consultation or intervention (n = 3), stroke (n = 1), and death (n = 2). Vascular injuries included 1 neck hematoma with superinfection requiring antibiotics, 1 neck hematoma requiring otolaryngology and vascular surgery consultation, and 1 venous dissection of IJ vein requiring vascular surgery consultation. None of these cases required operative intervention. The stroke was caused by inadvertent CVC placement into the carotid artery. One patient experienced tension pneumothorax and died due to this complication; this death occurred after 3 failed left subclavian CVC attempts and an ultimately successful CVC placement into left IJ vein. Another death occurred immediately following unsuccessful Cordis placement. As no autopsy was performed, it is impossible to know if the cause of death was the line placement. However, it would be prudent to consider this as a CVC complication given the temporal relationship to line placement. Thus, the total number of patients who experienced severe mechanical complications was 14 out of 730 (1.92%).