Qualitative assessment of organizational barriers to optimal lung cancer care in a community hospital setting in the United States
Background Lung cancer is a major public health challenge in the United States with a complicated process of care delivery. In addition, it is a challenge for many lung cancer patients and their caregivers to navigate health care systems while coping with the disease.
Objective To explore the organizational barriers to receiving quality health care from the perspective of lung cancer patients and their caregivers.
Methods In a qualitative study involving 10 focus groups of patients and their caregivers, we recorded and transcribed guided discussions for analysis by using Dedoose software to investigate recurrent themes.
Results Analysis of the transcriptions revealed 4 recurring themes related to organizational barriers to quality care: insurance, scheduling, communication, and knowledge. The participants perceived support with navigating the health care system, either through their own social network or from within the health care systems, as beneficial in coping with the lung cancer, seeking information, expediting appointments, connecting patients to physicians, and receiving timely care.
Limitations Institutional and geographic differences in the experience of lung cancer care may limit the generalizability of the results of this study.
Conclusions This study offers insights into the perspectives of lung cancer patients and caregivers on the organizational barriers to receiving quality care. Targeting barriers related to insurance coverage, appointment scheduling, provider-patient communication, and patient or family education about lung cancer and its treatment process will likely improve patient and caregiver experience of care.
Funding Partially funded through a Patient-Centered Outcomes Research Institute Award (IH-1304-6147).
Accepted for publication March 2, 2018
Correspondence Raymond U Osarogiagbon, MBBS; rosarogi@bmhcc.org
Disclosures The authors report no disclosures/conflicts of interest.
Citation JCSO 2018;16(2):e89-e96.
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0394
Submit a paper here
Results
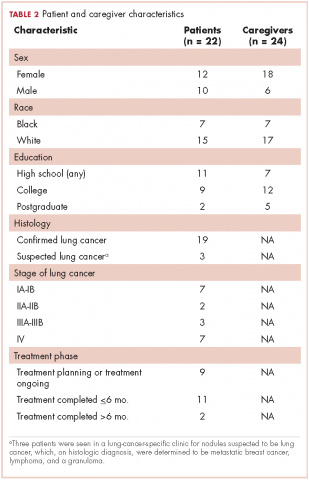
The 10 focus groups included 46 participants: 22 patients and 24 caregivers (some patients brought multiple caregivers). Of the 22 patients, 12 were women and 7 were black. An equal proportion of patients had at least a high school education as had a college or postgraduate degree. Although all of the patients had had a lung lesion suspicious for lung cancer, 19 eventually had a histologic diagnosis of lung cancer. The remaining 3 patients were all evaluated in a thoracic oncology clinic but were eventually found to have metastatic breast cancer, lymphoma, and a granuloma. Nine patients were either currently in the treatment decision-making process or actively receiving treatment, 11 had completed treatment within the preceding 6 months, and 2 had completed treatment more than 6 months previously. Treatment covered the spectrum from curative intent to palliative care. Of the 24 caregivers, 18 were women and 7 were black; 12 caregivers had at least a college education, of whom 2 had postgraduate degrees (Table 2).
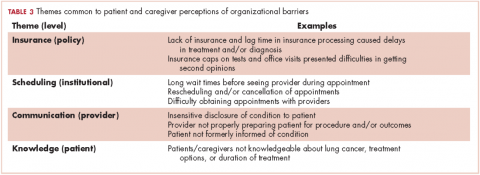
Based on participants’ feedback, we identified 4 main levels within the system where barriers to optimal care occurred: policy, institutional, provider, and patient. From our qualitative analyses, we identified a central theme associated with each level, around which the barriers coalesced. The themes were insurance, scheduling, provider communication, and patient knowledge. At the policy level, medical insurance was perceived to affect the timeliness of care and to be a deterrent to timely diagnosis and quality treatment. Lack of insurance was a daunting obstacle for indigent patients. However, even those who were insured felt that dealing with insurance companies was a significant barrier to care. At the institutional level, appointment scheduling caused problems for both patients and their caregivers. At the health care provider level, communication was perceived as a major problem. And finally, at the patient level, both patient and caregiver lack of knowledge of lung cancer and the processes inherent in lung cancer treatment were barriers for optimal diagnosis and treatment (Table 3).
,
Insurance barriers
At the policy level, health insurance was reported as a significant barrier to accessing health care. Patients and caregivers reported delays in diagnosis and/or treatment because of either lack of insurance or lag time in insurance processing of clinician requests. Insurance restrictions on tests, procedures, and office visits presented difficulties in getting additional opinions from providers regarding diagnosis, prognosis, or treatment plans. Some patients were no longer able to see providers after they had met the test or office visit limit allotted by insurance providers. One patient shared the following experience with office visits leading up to their lung cancer diagnosis:
Patient … with my insurance I just had only 12 office visits … and I had already maxed those out.
In other instances, insurers would not cover hospital or clinic visits if certain logistic protocols were not met. This would sometimes leave patients stranded for a period of time without receiving any care.
Caretaker … went home and went to one of those minor emergency clinics and they sent her to [xx hospital in another city]. There they did nothing. That was then over the weekend, and my son wanted to get her out of there to get her into practice because they weren’t doing anything. They said, ‘No. Your insurance won’t pay for it unless you stay here till we sign the papers to be transferred.’ … It was a bandage. Period.
Some insurers would not cover certain health services outside of routine testing protocols for the patients’ conditions. This lack of coverage caused patients to pay out of pocket for needed care.
Patient Nothing in the lymph nodes, but if it hadn’t been for me going ahead with this [coronary] calcium score, the insurance wasn’t gonna pay anything. If it wouldn’t been for the 79 bucks or the family situation, I wouldn’t be sitting [here] today.
Individuals who had not yet met the age requirement for Medicare reported being without insurance for a period of time, which contributed to delays in accessing care.
Caregiver [xx patient] probably … could’ve been diagnosed maybe even months ago, but she is in that in-between where she gets Social Security but she’s not 65 until November, so she has no insurance.
Scheduling barriers
At the institutional level, patients and caregivers reported problems with appointment scheduling. Logistic problems with adjusting work schedules and arranging for transportation as well as long wait times before evaluation by a provider were recurrent themes expressed by both patients and caregivers. Many had become resigned to the expectation of long wait times during appointments.