Calculating Risk for Poor Outcomes After Transcatheter Aortic Valve Replacement
The decision of selecting SAVR over TAVR is typically driven by factors other than short- or long-term mortality (eg, whether TAVR will be covered by insurance, very young age and concern about durability, need to treat concomitant mitral regurgitation or aortopathy), as clinical trials have shown that survival and quality of life outcomes are at least as good with TAVR compared with SAVR.6,7,9,23 In fact, in an analysis that compared similar patients treated with TAVR versus SAVR and specifically looked for patient factors that might make one treatment preferable to the other, patients who had a prior cardiac operation and those on home oxygen were more likely to do better with TAVR, whereas no patient factors that favored SAVR were found.24 The majority of patients, however, were expected to have similar long-term outcomes regardless of treatment choice, and as such, the benefit of TAVR appears mostly to be an earlier and easier recovery.
Long-Term Outcomes: Estimating the Risk for Failure to Recover
While many patients who undergo TAVR are quite ill prior to the procedure, with substantial limitations due to the fatigue and shortness of breath associated with severe aortic stenosis, most patients recover well after the procedure, with marked improvement in symptoms and functional capacity. Approximately 25% to 35% of patients currently treated with TAVR commercially (ie, intermediate- and high-surgical-risk patients) either die or do not recover a reasonable quality of life after the procedure. Identifying those patients prior to the procedure can be challenging. We have previously developed and externally validated
Beyond clinical factors, frailty negatively impacts both survival and quality of life after TAVR. Frailty is a geriatric syndrome of impaired physiologic reserve and decreased resistance to stressors27 that is characterized by weakness, slowness, exhaustion, wasting, and low activity level. Across a wide variety of clinical situations (eg, pneumonia,28 myocardial infarction,29 general30,31 and cardiac surgery32,33), frailty increases the risk of morbidity and mortality after nearly any intervention34 or clinical insult, independent of traditional demographic and clinical risk factors. Frail patients often do better with less invasive interventions such as TAVR compared with traditional surgery, but nonetheless remain at increased risk for death35-37 or failure to recover quality of life and functional status25,37 after TAVR. However, there are unique challenges in both assessing and managing frailty in patients who are considered potential candidates for TAVR. One challenge is the lack of a laboratory or radiologic test for frailty; instead, the lack of physiologic reserve of frailty is identified through a combination of factors, such as slow gait speed, weak grip strength, and unintentional weight loss. While these factors readily identify frail patients in general elderly populations, in patients with severe symptomatic aortic stenosis, these metrics can be impacted by the disease process itself. This distinction is important as slow gait speed that is due to aortic stenosis will be “fixed” by TAVR, but slow gait speed from frailty would identify a patient who will have a difficult time recovering from the procedure. For example, in the CoreValve High Risk Pivotal Trial, 80% of patients had a slow gait speed and 67% had a weak grip strength,5 and yet 58% of patients in this trial were alive and with a reasonable quality of life 1 year after TAVR.6 A number of studies have attempted to define true frailty within the pre-TAVR population, that which represents decreased physiologic reserve and an impaired ability to recover from an insult, and the factors that appear to be most prognostically important are malnutrition38 or unintentional weight loss25 and the inability to be independent in activities of daily living (eg, dressing, feeding, transferring).25,37
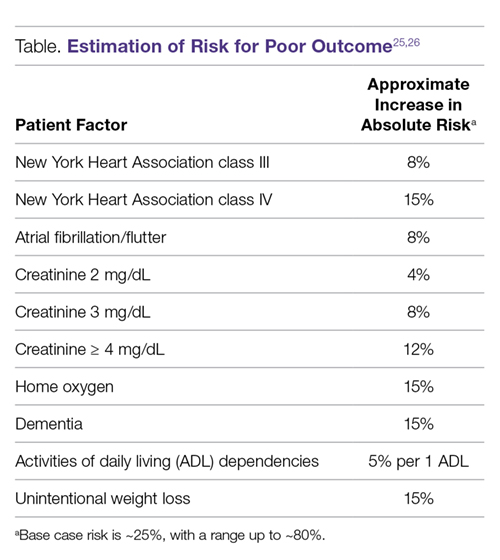
Even with frailty assessments, the ability to predict who is or is not going to have a poor outcome after TAVR (ie, to use pre-procedural factors to identify patients who perhaps should not be offered TAVR because he or she will not recover from the procedure) is exceedingly difficult. The Table shows how to grossly estimate risk using the major factors that impact risk based on the more precise estimates from our models.25,26
The model shown in the Table can be used to estimate a patient’s risk for a poor outcome, but it should be noted that even at the extreme high end of risk, there will be some patients who still do well after TAVR. Furthermore, being high risk for a poor outcome after TAVR does not imply anything about how the patient would do without TAVR, as many of these patients would likely die even sooner or have worse quality of life with medical therapy only. However,
Conclusion
Calculating the risk of TAVR can be complicated. In patients who are electively treated using transfemoral access and a less invasive approach, the short-term risk of mortality is very low. Risk calculators can be used to estimate short-term risk, but the patients who are high risk for in-hospital mortality are often fairly easy to recognize, as the factors that drive that risk are not subtle (eg, the patient is in shock at the time of the procedure). The true risk of TAVR lies in the inability to recover from the procedure—being chronically ill, frail, or debilitated to a degree that the patient either dies or fails to recover a reasonable quality of life. Given
Corresponding author: Suzanne V. Arnold, MD, MHA, 4401 Wornall Rd., Kansas City, MO 64111.
Financial disclosures: This work was funded in part by grant K23HL116799 from the National Institutes of Health.