Health Care–Associated Urinary Tract Infections: Prevention and Management
Catheter-Associated UTI in Patients with Spinal Cord Injury
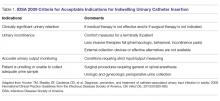
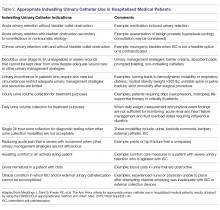
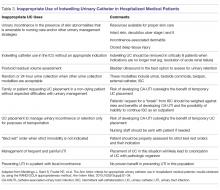
Spinal cord injury (SCI) at any level can cause neurogenic bladder. This process ultimately leads to urinary stasis and colonization of the bladder with bacteria. According to the IDSA, the acceptable indications for UC insertion are: clinically significant urinary retention (if medical therapy is not effective), urinary incontinence, accurate urine output monitoring required, and patient is unable and/or unwilling to collect urine (Table 1).5 Recently, further guidelines were published regarding appropriate and inappropriate indwelling UC placement in hospitalized medical patients (Table 2 and Table 3), expanding upon the earlier acceptable criteria provided by the IDSA.41 According to the IDSA and Ann Arbor Criteria for Appropriate Urinary Catheter Use, patients with SCI and subsequent neurogenic bladder without obstruction where intermittent bladder straight catheterization for the drainage of urine is not feasible will likely need an indwelling UC.41 SCI patients often experience decubitus ulcers, and an indwelling UC can be used if needed to help with wound healing if other urinary management alternatives have been attempted. Other such situations in which an indwelling UC can used before attempting alternative approaches would be in a patient who is actively dying and is pursuing comfort care and/or hospice.41
Which indwelling UCs should be used in patients with SCI?
Efforts to reduce the likelihood of infection in patients with SCI have led to several advances in the design and manufacturing of UCs. UCs are made of either latex, plastic, silicone, or polytetrafluoroethylene (Teflon). None of these substrates is free of complications, but of them latex UCs have been studied the most in regards to their associated complications. Aside from being allergenic in nature, latex UCs have an increased propensity to allow bacteria to adhere to their surface due to microscopic planes of unevenness.42 Silicone UCs are less frequently associated with infection but are more rigid, leading to increased discomfort.43,44 Hydrophilic and silver-hydrogel coatings are innovative methods that have been developed to increase comfort and reduce the likelihood of infection. Hydrophilic-coated UCs are associated with reduced microbial adherence, decreased encrustation, and better patient satisfaction.45,46 In SCI patients, these UCs have demonstrated lower complication rates, including UTI; fewer episodes of post-, intra-, and inter-catheterization bleeding; and decreased rates of antibiotic-resistant bacteria.45,46 Silver-hydrogel-coated UCs are less well studied but have also demonstrated reduced UTI rates in SCI patients; however, their efficacy over the long term has yet to be determined. Antibiotic-impregnated UCs are not currently recommended for either short- or long-term indwelling UC use.5
How can CA-UTI be prevented in a patient who will require a long-term indwelling catheter?
At this time, the data is insufficient to make a recommendation on routine UC exchange (eg, every 2 to 4 weeks) in patients who require long-term indwelling urethral or suprapubic catheters in an attempt to reduce the risk of CA-ASB or CA-UTI. This is also true for those who experience even repeated early catheter blockage from encrustation.5 Thus, the rate at which these exchanges occur can be controversial, but typically around every 4 weeks is a common approach. Some would argue that if the patient has repeated CA-UTI, an exchange rate of every 2 weeks might be needed, but data is currently lacking to support this practice.5 If intermittent urinary catheterization is feasible, it should be done at least every 6 hours and before bedtime. In general, when the volume of urine in the bladder reaches approximately 400 mL, the patient should undergo bladder catheterization to prevent stasis and infection.47 A closed drainage system is recommended in all patients who require long-term indwelling UC use.48,49 Placement of the collection bag above the catheter or above the level of the bladder and a breach in the closed drainage system have been shown to result in higher rates of catheter-associated bacteriuria.48,50 Proper hand hygiene and sterile and/or clean techniques should be used when placing or exchanging a UC. However, in one study there was no difference in bacteremia or UTIs when using sterile versus clean techniques.51
Asymptomatic bacteriuria should not be treated in patients with long-term indwelling UCs, and prophylactic antibiotics have led to the emergence of resistance.52 At this time it is not clear whether prophylactic weekly oral cyclic antibiotic administration can effectively reduce the frequency of CA-UTI in patients with SCI and chronic indwelling UC use.
What are the signs and symptoms of CA-UTI in a patient with SCI?
Subjective and objective findings may be limited when a patient with SCI presents with CA-UTI. These patients often lack the usual symptoms of UTI (dysuria, suprapubic discomfort, urgency, increased frequency) and pyelonephritis (flank pain, costovertebral angle tenderness). Caregivers and health care providers should be aware that nonspecific symptoms such as foul-smelling urine, pyuria, increased residual volume of urine in the bladder, change in voiding habits, worsening detrusor spasticity, and aggravation of autonomic dysreflexia can be the only initial presenting symptoms.53