Outcomes After Endoscopic Dilation of Laryngotracheal Stenosis: An Analysis of ACS-NSQIP
From the Northwestern University, Feinberg School of Medicine, Chicago, IL (Mr. Bavishi, Dr. Lavin), the Johns Hopkins University, Baltimore, MD (Dr. Boss), Children’s National Medical Center, Washington, DC (Dr. Shah), and Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL (Dr. Lavin).
Abstract
- Background: Endoscopic management of pediatric subglottic stenosis is common; however, no multiinstitutional studies have assessed its perioperative outcomes. The American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS-NSQIP-P) represents a source of such data.
- Objective: To investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to those seen with open reconstruction techniques.
- Methods: Current procedural terminology (CPT) codes were queried for endoscopic or open airway reconstruction in the 2015 ACS-NSQIP-P Public Use File (PUF). Demographics and 30-day events were abstracted to compare open to endoscopic techniques and to assess for risk factors for varied outcomes after endoscopic dilation. Outcome measures included length of stay (LOS), 30-day rates of reintubation, readmission, and reoperation.
- Results: 171 endoscopic and 116 open procedures were identified. Mean age at endoscopic and open procedures was 4.1 (SEM = 0.37) and 5.4 years (SEM = 0.40). Mean LOS was shorter after endoscopic procedures (5.5 days, SEM = 1.13 vs. 11.3 days SEM = 1.01, P < 0.001). Open procedures had higher rates of reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009). In patients undergoing endoscopic dilation, children < 1 year were more likely to require readmission (OR = 4.21, P = 0.03) and reoperation (OR = 4.39, P = 0.03) when compared with older children.
- Conclusion: Open airway reconstruction is associated with longer LOS and increased reintubations and reoperations, suggesting a possible opportunity to improve value in health care in the appropriately selected patient. Reoperations and readmissions following endoscopic dilation are more prevalent in children younger than 1 year.
Keywords: airway stenosis; subglottic stenosis; endoscopic dilation; pediatrics; outcomes.
Historically, pediatric laryngotracheal stenosis was managed using open reconstruction techniques, including laryngoplasty, tracheal resection, and cervical tracheoplasty. Initial reports of endoscopic dilation were described in the 1980s as a means to salvage re-stenosis after open reconstruction [1]. Currently, primary endoscopic dilation has become commonplace in otolaryngology due to its less invasive nature as well as—in cases of balloon dilation—minimization of tissue damage [2]. The advancements made in endoscopic balloon dilation have reduced the frequency with which open reconstruction is performed.
Systematic reviews and case series investigating endoscopic dilation indicate a 70% to 80% success rate in preventing future open surgery or tracheostomy [2–5]. While increased severity of stenosis has been associated with poorer outcomes in endoscopic procedures, few other risk factors that influence surgical success have been identified [4,5]. In a single study in the adult literature, open surgical management of idiopathic subglottic stenosis was associated with improved outcomes when compared to endoscopic techniques [5]. Such findings suggest a need to identify these factors for the purpose of optimizing clinical decision-making.
As laryngotracheal stenosis is rare, postoperative outcomes and risk factors are best identified on a multiinstitutional level. Due to its participation from 80 hospitals and its accurate and reliable reporting of both demographic and risk-stratified 30-day outcomes data, the American College of Surgeon’s National Surgical Quality Improvement Program – Pediatric (ACS NSQIP-P) provides such a platform [6–8]. Thirty-day outcomes and risk factors for open reconstruction utilizing the ACS NSQIP-P database have previously been reported; however, no such outcomes for endoscopic dilation have been described, and no comparison between endoscopic and open procedures has been made [9]. The purpose of this study was to utilize the 2015 ACS-NSQIP-P database to investigate 30-day outcomes of endoscopic dilation of the pediatric airway and to compare these outcomes to open reconstruction techniques. Secondarily, we aimed to determine if any demographic factors or medical comorbidities are associated with varied outcomes in endoscopic reconstruction. While these data reflect safety and quality of this procedure in the United States, findings may potentially be applied across international settings.
Methods
Data Source
Data was obtained from the 2015 ACS-NSQIP-P Public Use File (PUF). Due to the de-identified and public nature of these data, this research was exempt from review by the Ann & Robert H. Lurie Children’s Hospital of Chicago review board. Data collection methods for ACS-NSQIP-P have previously been described [10]. In brief, data was collected from 80 hospitals on approximately 120 preoperative, intraoperative, and postoperative variables. Cases are systematically sampled on an 8-day cycle basis, where the first 35 cases meeting the inclusion criteria in each hospital in each cycle are submitted to ACS-NSQIP-P.
Variables and Outcomes
Airway procedures for endoscopic dilations and open reconstructions were obtained by CPT code. Endoscopic dilations (CPT 31528) were compared to open reconstructions, which included laryngoplasty (31580, 31582), cervical tracheoplasty (31750), cricoid split (31587), and tracheal resection (31780). Demographic variables included age, sex, race, and history of prematurity. Presence of specific comorbid diseases were also collected and tested for significance.
Dependent outcomes of interest were unplanned 30-day postoperative events grouped as reoperation, unplanned readmission, and postoperative reintubation. In the case of endoscopic procedures, the presence of salvage open reconstruction or tracheostomy within 30 days of surgery was also recorded. Length of stay (LOS) after the procedure was collected. Specific postoperative complications and reasons for readmission were recorded within the limitations of data available in the PUF.
Analysis
Analysis was performed using descriptive statistics and frequency analysis where appropriate. Chi-square analysis was used to compare adverse events between open and endoscopic procedures. Logistic regression with calculation of odds ratio (OR) was performed to determine predictive factors for reoperation, readmission, and reintubation in all pediatric airway reconstructive procedures in adjusted and unadjusted models. T-test and linear regression was performed on the continuous outcome of length of stay. For all analyses, a p value of < 0.05 was considered statistically significant. All variable recoding and statistical analyses were performed in SAS/STAT software (Cary, NC).
Results
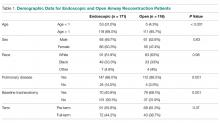
A total of 84,056 pediatric procedures were extracted from the 2015 NSQIP-P PUFs. Using the above CPT codes, 171 endoscopic dilations and 116 open airway reconstructions were identified, with patient age ranging from 0 days to 17.6 years. Average age of patients undergoing endoscopic dilation and open reconstruction was 4.1 and 5.4 years, respectively (Table 1).
Potential confounders were tested with univariate logistic regression to determine if they had a significant impact on readmission, reintubation, or reoperation rates. These variables (Table 2)
In patients undergoing endoscopic dilation, average length of stay was 5.5 days (SEM = 1.13), with 79 (48.5%) patients having a length of stay of zero days. Of all patients who had endoscopic dilations, 70 (40.1%) had a pre-existing tracheostomy and these accounted for the majority (73%) of patients who had zero days as their LOS. LOS after endoscopic management was significantly shorter than the mean of 11.3 days (SEM = 1.01) reported in those undergoing open reconstruction (P < 0.001).
With respect to 30-day adverse events, 2 patients in the endoscopic group (1.1%) required reintubation. Thirteen endoscopic dilation cases (7.6%) had an unplanned readmission, four (2.3%) of which were associated with reoperation within 30 days of the primary surgical procedure. There were 9 other reoperations unassociated with unplanned readmission. Three of these reoperations were due to failed endoscopic dilations, resulting in 2 tracheostomies and one open airway reconstruction. There was one patient death, in a 0-day old with tetralogy of Fallot, trachea-esophageal fistula, and ventilator dependence who underwent emergent endoscopic dilation and died the same day.
Open procedures were associated with 11 unplanned readmissions (9.5%), 7 re-intubations (6%) and 18 reoperations (15.5%). Of patents undergoing reoperation, one patient undergoing open reconstruction underwent tracheostomy within 30 days of surgery.
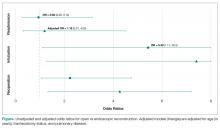
When comparing open reconstruction to endoscopic dilation, there was a significant increase in reintubation (OR = 7.41, P = 0.026) and reoperation (OR = 3.09, P = 0.009) for open procedures, even with adjustment for age, tracheostomy status, and pulmonary disease. There was no significant difference between the two for unplanned readmissions (OR = 1.19, P = 0.79) (Figure
Younger age was also found to be significantly associated with reoperation rates, in an adjusted logistic model that accounted for tracheostomy status, type of surgery, and pulmonary disease. Per year of life, younger children had higher reoperation rates than older children (OR = 1.91, P = 0.017). When endoscopic dilation was individually examined, children younger than 1 year of age were more likely to undergo reoperation after an endoscopic dilation than children older than 1 (OR = 4.39, P = 0.03). Children under age 1 were also more likely to have an unplanned readmission after an endoscopic dilation (OR = 4.21, P = 0.03). The relationship between age and re-intubation was not significant (OR = 0, P = 0.95). For open reconstruction, this age dichotomization was not associated with any increased reoperation (OR = 2.3, P = 0.52), readmission (OR = 0, P = 0.97), or reintubation (OR = 0, P = 0.94).
T-test analysis was performed to determine if children < 1 year old also had significantly longer hospital stays after endoscopic dilation than older children (mean 14.1 days vs 1.9 days, P < 0.001). This relationship held true in a linear regression after adjustment for pulmonary disease and tracheostomy, with length of stay decreasing by 0.48 days per year of life (P = 0.03). For endoscopic dilations, the same relationship held true, where length of stay decreased by 0.75 days per year of life.