A Multipronged Approach to Decrease the Risk of Clostridium difficile Infection at a Community Hospital and Long-Term Care Facility
Journal of Clinical Outcomes Management. 2015 September;SEPTEMBER 2015, VOL. 22, NO. 9:
September 2, 2015|Journal of Clinical Outcomes Management
Antibiotic Pressure
Certain antibiotic classes have been more associated with increased CDI risk. Antibiotics preceding each CDI infection are noted in Figure 4. The data shows that proportionally more patients with CDI received fluoroquinolones as the preceding antibiotic, followed by third- or fourth-generation cephalosporins, extended-spectrum penicillins, and the carbapenem class. Some antibiotics were
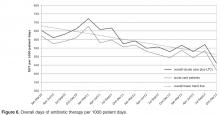
implicated simply by being combined with another higher risk class of antibiotics, eg, aminoglycosides. Our antibiotic stewardship program led to the streamlining of antibiotic therapy and reduced utilization of broad-spectrum antibiotics (Figure 5). Patient days of antibiotic therapy per 1000 patient days were used for
trending antibiotic use. Since we began tracking this in 2010, we have seen a 30% reduction in overall days of therapy (Figure 6). Multiple antibiotic courses also had a significant association with PPI administration in the patients who contracted CDI (chi square = 6.9, df = 1, P = 0.009, OR 2.94).
Acid Suppression
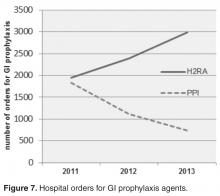
In evaluating the effects of limiting the use of PPIs, patients who received an H2RA or no antacid prophylaxis were significantly less likely to have a recurrence of CDI than those who received a PPI (chi square = 6.35, df = 1, P = 0.012). The OR for recurrence with PPIs was 3.05 (95% CI 1.25 to 7.44). Of patients exposed to PPIs, those exposed in the later time period (2011 through 2013) were significantly less likely to have a recurrence than those exposed in the early time period (third quarter 2008 through 2010; chi square = 15.14, df = 1, P < 0.001). The OR was 0.23 (95% CI, 0.11 to 0.49).
As seen in Figure 2, the number of CDI events declined markedly over the first 2 years then plateaued or very slowly declined for the remainder of the study. As seen in Figure 7, the use of PPIs continued to decline, and the use of H2RAs continued to increase from 2011 on. Initially, in 2009, 95% of CDI cases were on a PPI, but by 2010 the rate of PPI use was declining rapidly at our facility, with only 55% of the CDI patients on a PPI, and 48% on an H2RA.