Enhancing the Communication Skills of Critical Care Nurses: Focus on Prognosis and Goals of Care Discussions
IMPACT-ICU Workshop
A maximum of 15 nurses participate in each 8-hour workshop. The session begins with introductions and small group discussions about what the participants perceive to be the greatest barriers to goals of care discussions and fostering patient/family decision-making in the ICU. Participants are also asked to reflect on what they want to learn as a result of their workshop attendance.
A short didactic session then reviews the definition of palliative care and its core components, addresses the nurses’ role in communication within palliative care, a social worker’s perspective of what it is like to be a family member in the ICU, and the outline of the day. This includes delineation of expectations for involvement within the role plays and the various roles to be enacted. An emphasis is placed on the workshop being a safe place to explore and trial skills with the support of colleagues, and that practice is the optimum way to integrate communication expertise into the nurses’ skill set.
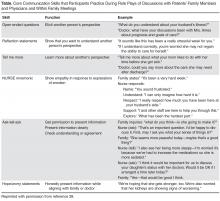
The “4 Cs” serves as the instructional basis for nurse communication skill enhancement [27]. This model outlines 4 key nursing roles in optimizing communication within palliative care:
Convening: Making sure multidisciplinary patient/family/clinician communication occurs.
Checking: Identifying the patient and family needs for information; ensuring that patients and families clearly receive desired information; ensuring that clinicians understand patient and family perspectives.
Caring: Naming emotions and responding to feeling.
Continuing: Following up after discussions to clarify and reinforce information and provide support.
Sample Role Play
Facilitator: So our first role play is focused on eliciting patient and family perspectives and needs. I need a learner and someone to play the role of the family member.
Learner: I’ll give it a try.
Facilitator: Lisa, you’re going to do great. Who wants to play the family member?
Workshop Participant: I’ll do it.
Facilitator: So Mary (who has agreed to play the role of the wife), why don’t you read us the scenario. (She reads it out loud to the group).
Facilitator: Lisa, as the nurse, I want you to look at your guide and tell me what your goal is for this conversation with Mrs. Ames and then which skill you want to practice.
Learner: I think I want to try eliciting the patient and family’s needs for information and I’ll try “Tell Me More” statements.
Facilitator: Alright. So remember Lisa, if you feel the conversation isn’t going well, you can call a “time out.” I can do this as well if I feel you need to start over. I’ll also call a time out when I feel you have met your goal. Sound OK? Mary, do you have any questions playing the part of Mrs. Ames?
Wife Role: Well, how hard should I make this for her? Should I be one of those “difficult” family members?
Facilitator: Our goal here is not to “stump” you or make it particularly difficult. We want you to try out these skills and get a sense of your “comfort zone.” So let’s start with some basic communication skills, OK?
Wife Role: Alright.
Facilitator: Why don’t we set the stage, such that Lisa, you are Mr. Ames’ nurse assessing him at the start of your shift, when Mrs. Ames enters. This is the first time you have taken care of him. The night nurse has told you that he has been requiring increasing ventilator support and his renal function is declining. Per Mrs. Ames’ request, the night nurse called her to let her know how he was doing and Mrs. Ames told her she would be in shortly.
Wife Role: (nervously enters the room and grasps her husband’s hand and looks at the nurse). How’s he doing? Is he better? The night nurse called me and I was so worried I rushed over here.
Learner: (Turns to Mrs. Ames and extends her hand). Are you Mrs. Ames? I’m Lisa and I am going to be taking care of Mr. Ames today. Let me just finish my assessment and how about we talk then? Will that be OK? It will be just a few minutes.
Wife Role: Alright, I’ll be in the waiting area but please come get me as soon as you can.
Learner: I will. (Nurse then shortly comes into the waiting area and asks Mrs. Ames to come back into the ICU where she invites her to sit just outside Mr. Ames’ room). Mrs. Ames, how are you doing? This must be so stressful for you, having your husband in the ICU.
Wife Role: It’s awful. He’s never been in the hospital before this and look at him, all hooked up to machines. I’m so worried. He seems to be getting worse instead of better.