The Co-design Event
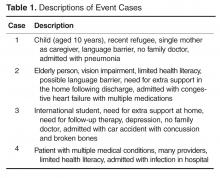
For the co-design event we created 4 patient cases that highlighted common factors that may complicate a discharge transition home, namely: patient age (pediatric and elderly patients), language barriers, limited health literacy, multiple health conditions, multiple medications, lack of a primary care doctor, and multiple follow-up visits (Table 1). The event had 21 attendees and 2 facilitators; details of the attendee composition and demographics are provided in Table 2. Participants in the design event were divided into 4 teams, and each team had a minimum of 1 patient, 1 provider, and 1 designer. Each team had 25 minutes per case to create a PODS for each of the 4 cases, and there were no other rules.
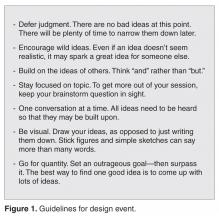
To ensure a spirit of open-mindedness and collaboration during the event, we used strategies outlined in the Design Thinking for Educators Toolkit to guide the process (Figure 1) [9]. Following the event, all participants were asked to complete an evaluation form where they had the opportunity to relay any information they did not have a chance to share during the event.
Solutions resulting from the design event ranged from more traditional discharge summaries that were enhanced with multiple languages and images to make things clear for patients, to solutions including interactive patient portals. There were solutions that came with stickers to color-code your medications, areas for patients to write notes, and checklists for them to keep track of all their follow-up plans.
The output included key information for patients such as phone numbers of who to call with questions and expectations for the first week home from the hospital. Almost all solutions contained a calendar view. Figure 2 shows a sample of the draft PODS created by the teams during the event. Details on the specific elements the participants suggested including in the PODS are listed in Table 3.
Refining the Design Using Focus Groups and Surveys
The ideas and concepts generated during the design event were analyzed by the interdisciplinary advisory team at OpenLab. In addition, several team sessions were held with health care
providers who attended the design event and who worked in local hospitals to determine feasibility of the PODS. Based on the results of the co-design event and literature review, a designer created the first PODS prototype (Figure 3).
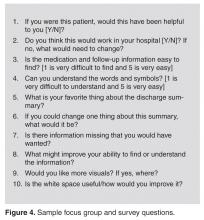
Using the first prototype and a sample case study, we held a series of focus groups and conducted 2 online surveys to get feedback on how the prototype could be further improved. Focus groups were held deliberately with harder-to-reach patient groups that do not typically provide input (eg, patients with extreme language barriers), and surveys were used to reach a broader and larger audience of patients and caregivers (Table 4). Figure 4 provides a sample of questions asked. The first prototype was then revised based on what we learned from the focus groups and surveys to create the second prototype (Figure 5). Table 5 provides the output from the focus groups and surveys that influenced the changes that were made to the first prototype. In all cases, the groups (see Table 4) that provided specific feedback is indicated. Most of the feedback from the focus groups and surveys was positive. All patients noted that they would love to receive a PODS
and would find it useful when they are discharged from hospital. A patient's comment:
This is a great piece. You guys are doing an awesome job. This would have saved me so much anxiety and fear of doing something wrong when I was discharged. I didn’t want to bother my doctors and went on a hope and prayer. Even my home care people weren’t always sure of what to do. Again this would be a great step forward in easing patients’ fears, especially senior citizens. GREAT WORK. THANKS FOR CARING.
Discussion
Innovative methods such as co-design events and targeted focus groups are very useful for
engaging patients and caregivers in the design and development of solutions aimed at improving their experience of care, resulting in solutions that are more successful. It is important to include all users, especially those who are harder to reach, such as patients with language barriers and mental health conditions. In addition,
engaging health care providers is essential to ensure feasibility of those solutions. During the co-design process, it was difficult to truly engage harder-to-reach patient populations. At first, we tried using traditional methods of engagement such as approaching patient advisory boards and posting flyers for focus groups; however, although patients agreed to participate, very few had extreme language barriers or limited health literacy. As such, considerable time and effort was made to target harder-to-reach patients by enlisting interpreters, having flyers translated, and offering incentives. Additionally, we made use of ongoing patient meeting groups of patients with mental health issues and had health care providers screen patients for limited health literacy.
Future Plans
The PODS template has now been adapted and implemented in several hospitals in Toronto, Canada, using a supported early adopter process [10]. Future plans are to test the impact of the PODS on patient experience and health outcomes using a randomized controlled trial. Also, for now, we have focused on a paper version of PODS, but with the increasing prevalence of electronic health records and consumer-oriented health care apps, future consideration for a digital and mobile version of PODS is warranted.