Patients, Persistence, and Partnership: Creating and Sustaining Patient and Family Advisory Councils in a Hospital Setting
From the Center for Patients and Families (Dr. Fagan, Ms. Wong, Ms. Morrison, Ms. Carnie), and the Division of Women’s Health and Gender Biology (Dr. Lewis-O’Connor), Brigham and Women’s Hospital, Boston, MA.
Abstract
- Objective: To describe and illustrate the phases of creating, recruiting, launching, and sustaining a successful Patient and Family Advisory Council (PFAC) in a hospital setting.
- Method: Descriptive report.
- Results: There are 4 stages in creating and establishing a PFAC: council preparation, patient/family advisor recruitment, council launch, and sustaining an established council. Each stage poses challenges that need to be addressed in order to progress to the next stage. The ability for hospital leadership to authentically partner with patient and family advisors is key to maintaining and sustaining PFACs.
- Conclusion: The success of a PFAC is based on leadership support, advisors’ commitment to their PFAC, and the ability to sustain the council. PFACs can promote patient- and family-centered care and shift the model of care from a prescribed model to one that embraces partnerships with patients while advancing care delivery. As patient- and family-centered care advances, it is important that best practices and resources for building and sustaining PFACs are developed and made available to ensure all hospitals have access to this valuable resource.
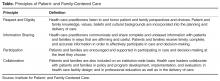
Throughout the country, families, patients, and health care professionals are working together in new ways, including within patient and family advisory councils (PFACs). First established in the 1990s, PFACs became widespread after patient-centeredness was identified by the Institute of Medicine as one of the 6 aims of quality health care [1]. PFACs were created to institutionalize a partnership between hospital leadership, clinicians, patients, and families to improve care delivery. Through this partnership, PFACs facilitate the sharing of patient perspectives and input on hospital policies and programs; serve as a resource to providers; and promote relationships between staff, patients, and family members [2]. PFACs also play an important role in promoting patient- and family-centered care, ensuring that patient needs and values are at the center of the care delivery system.
The BWH Center for Patients and Families includes the executive director, a project manager, and a senior patient advisor, who together oversee the PFACs. The project manager provides logistical support and is available as concerns arise, working closely with the senior patient advisor to ensure patient/family advisors are acclimated to their role and all PFACs run smoothly. The senior patient advisor is a volunteer advisor and patient advocate with long term experience creating and sustaining PFACs and mentoring patient/family advisors. Her role as a mentor includes attending PFAC meetings to model skills and behaviors for other advisors and working with them to ensure they are comfortable in their PFAC. Her advocacy work includes listening to and helping to articulate lived patient/family experiences as compelling narratives, which can be shared with hospital leadership and used as exemplars to spur change. Together, the team recruits and trains patient/family advisors, support all phases of PFAC development, and represent the patient/family voice within the hospital.
In this article, we describe and illustrate the 4 stages of creating and sustaining a successful PFAC to provide guidance and lessons learned to organizations seeking to develop this valuable resource. These stages are: (1) council preparation, (2) patient/family advisor recruitment, (3) council launch, and (4) sustaining an established council.