Symptomatic Intracranial Atherosclerotic Disease
Further Evaluation
What imaging is recommended to identify patients with ICAD?
The Stroke Outcomes and Neuroimaging of Intracranial Atherosclerosis (SONIA) trial sought to evaluate the reliability of noninvasive imaging modalities to identify a 50%–99% stenosis of large proximal cerebral arteries as compared with the gold standard of conventional angiography [3]. Qualifying vessels included the M1 segment of the middle cerebral artery, the carotid siphon, and intracranial vertebral and basilar arteries. Imaging techniques included MRA head without contrast (time of flight) and TCD ultrasound. Both of these imaging modalities demonstrated a high negative predictive value (NPV) for the presence of a 50%–99% intracranial stenosis; however, the positive predictive value (PPV) for TCD and MRA was only 55% and 66%, respectively. Subsequent studies of contrast-enhanced MRA and CTA of the headhave shown high PPV (78%–94%) and NPV (95%–100%) when compared with cerebral angiography for the detection of 70%–99% ICAD [4,5]. Together these data suggest that TCD and MRA of the head without contrast can be used as screening tools to rule out ICAD when normal; however, subsequent contrast-enhanced MRA or CTA is required when abnormalities are identified.
When choosing the best noninvasive imaging modality for any given patient, concomitant medical issues including renal disease, age, presence of a pacemaker, implantable cardiac defibrillator or other metal, and claustrophobia are factors to consider.
What are the potential mechanisms of ischemic stroke in patients with symptomatic ICAD?
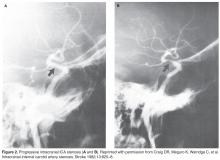
Stroke in the symptomatic ICAD group occurs as a result of either (1) thrombus formation at the site of a high-grade stenosis due to an unstable atherosclerotic plaque, (2) low flow through a narrow, stenotic artery (hypoperfusion) or (3) a combination of atheroembolism and hypoperfusion [6]. While a thrombus can occlude the parent vessel at the site of stenosis, more commonly the thrombus migrates distally as an artery-artery embolism to a smaller caliber artery.
What medical regimen is recommended for this patient with symptomatic ICAD?
Dual Antiplatelet Therapy
DAT with aspirin and clopidogrel is thought to reduce ischemic events related to regional thromboembolism. The best clinical evidence of the use of DAT in symptomatic ICAD is found in outcomes data for the SAMMPRIS trial where 30-day recurrent ischemic stroke rates in the aggressive medical management arm were significantly lower than patients treated with aspirin or warfarin monotherapy as part of the Warfarin and Aspirin for Symptomatic Intracranial Arterial Stenosis (WASID) trial. A subgroup of patients enrolled in WASID with similar clinical characteristics to those in SAMMPRIS were found to have a 30-day rate of stroke or death of 10.7% and a collective 1-year rate of ischemic stroke, brain hemorrhage, or vascular death of 25% [2]. The corresponding rates in the SAMMPRIS medical management arm were 5.8% at 30 days and 17.5% at 1 year. Given that the recurrent stroke rates were significantly lower in as little as 30 days, these benefits have been hypothesized to be more likely secondary to the DAT regimen than other risk factor modification [7]. There is some evidence that longer term DAT with aspirin and clopidogrel up to 1 year may be associated with further reduction in stroke, MI, and vascular death with similar bleeding risk, but this needs to be evaluated in prospective studies [8].
Additional evidence of the benefit and potential mechanism from DAT in ICAD comes from CLAIR (Clopidogrel plus Aspirin versus Aspirin alone for Reducing Embolization in Patients with Acute Symptomatic Cerebral or Carotid Artery Stenosis Trial), a multicenter, randomized trial with blinded outcome assessment, with patients recruited at sites in Hong Kong, Singapore, China, Thailand, and Malaysia [9]. Patients were enrolled with an extracranial or intracranial stenosis (greater than or equal to 50%, as diagnosed by carotid duplex, transcranial Doppler, or magnetic resonance angiography) if they had a clinical diagnosis of acute ischemic stroke or transient ischemic attack (TIA) during the 7 days prior to enrollment and were found to have microembolic signals (suggesting microemboli of atherosclerotic origin) detected at baseline assessment with transcranial Doppler ultrasound. Patients were randomized to DAT with aspirin and clopidogrel versus aspirin monotherapy. Patients on DAT had significantly reduced microembolic signals compared with patients on aspirin monotherapy. Asymptomatic embolization with dual antiplatelet therapy may also proffer a reduction in clinical events in these patients with symptomatic ICAD.
Statin Therapy
Statin therapy is an integral part in the prevention of recurrent ischemic events in the symptomatic ICAD cohort. Post-hoc analyses from the WASID trial found that total cholesterol greater than 200 mg/dL was associated with an increased risk of ischemic stroke, myocardial infarction, or vascular death.
In 2013, the American Heart Association released new guidelines regarding the treatment of cholesterol to reduce atherosclerotic cardiovascular risk in adults [10]. Clinical atherosclerotic cardiovascular disease (ASCVD) is the manifestation of systemic atherosclerotic disease and defined as acute coronary syndromes, a history of myocardial infarction, stable or unstable angina, a history of coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease presumed to be of atherosclerotic origin. Recommendations for secondary prevention in patients with clinical ASCVD include the use of high-intensity statin therapy (atorvastatin 40 or 80 mg, rosuvastatin 20 or 40 mg) for patients less than 75 years of age or moderate-intensity statin therapy (atorvastatin 10 or 20 mg, rosuvastatin 5 or 10 mg, pravastatin 40 mg, or simvastatin 20 or 40 mg) for patients > 75 years of age. In the SAMMPRIS trial, an LDL cholesterol level less than 70 mg/dL was targeted [7].