Patient-Physician Communication and Diabetes Self-Care
From the Department of Family Medicine (Dr. Beverly) and the Department of Medicine (Mss. Worley, Court, Prokopakis, and Ivanov), Ohio University Heritage College of Osteopathic Medicine, Athens, OH.
Currently, 3 ongoing studies aim to improve self-care and clinical outcomes via physician-patient communication interventions. A study by Ricci-Cabello and colleagues [103] aims to improve diabetes self-care by enhancing patient-physician communication in an underserved community of adults with uncontrolled type 2 diabetes. In this 3-arm randomized controlled trial, patients allocated to groups A and B received communication skills training and graphic feedback about glycosylated hemoglobin A1c levels; patients in group C received usual care. Patients in group B also received telephone reinforcement [103]. The second study, by Billimek and colleagues, aims to improve physician-patient communication about medication regimens via diabetes coaching [104]. In this intervention, 190 Mexican-American adult patients with type 2 diabetes were randomly assigned to complete a Coached Care visit with trained community health workers or a Coached Care visit plus the EMPATHy software toolkit, a computer-based activity with strategies and resources to overcome self-care barriers. The primary endpoints are (1) the development of care plan that addresses everyday barriers to medication adherence and (2) completion of a concrete behavioral goal [104]. Finally, the third study, by Grant and colleagues, aims to improve physician-patient communication via a pre-visit prioritization of diabetes concerns. In this controlled, cluster-randomized, multisite trial, primary care physicians were randomized to the Pre-Visit Prioritization for Complex Patients with Diabetes or the control group [105]. The Pre-Visit Prioritization IT-tool is designed to help patients identify one or two concerns prior to a medical visit and then send these priorities to the primary care physician via an electronic health record. The overall goal of the intervention is to improve communication of self-care concerns during a medical visit [105]. Findings from these 3 interventions are forthcoming; findings may provide evidence for validated interventions that improve physician-patient self-care communication in diabetes.
Techniques to Improve Self-Care Communication
Incorporating communication skills in continuing medical education and diabetes education may improve self-care communication in the physician-patient relationship. Educational programs that teach physicians how to provide consistent messages, repeat information, reinforce and offer feedback regarding specific self-care behaviors, and problem-solve self-care challenges may improve patients’ willingness to discuss self-care [14,106]. Most patients will remember only a small portion of the information given to them during medical visit. Studies that compare how much information patients retain versus how much information physicians provide show that patients forget 31% to 71% of information [107]. Therefore, physicians need techniques that promote open self-care communication during a visit. The following techniques can help physicians improve self-care communication [108]:
- Discuss the most important self-care information first; patients tend to remember the information that is presented first.
- Use the phrase “This is very important…” when discussing key points because patients will remember things that are perceived as important.
- Deliver simple, clear, and concrete instructions; patients are more likely to forget complex or confusing instructions. For example, “Check your blood glucose every morning within five minutes of waking up and before you eat breakfast” is more specific and easier to follow than “Check your blood glucose”.
- Ask open-ended questions to allow patients to verbalize feelings or concerns about their diabetes self-care.
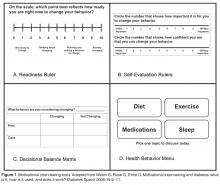
- Employ MI techniques to help patients who are struggling to initiate and adhere to self-care behaviors. MI tools, such as the Readiness Ruler, Self-Evaluation Rulers, Decisional Balance Matrix, and Health Behavior Menu (Figure), may help patients and physicians discuss self-care behaviors during a medical visit [109].
– Express empathy by reflective listening and asking patients for permission before offering information or advice about diabetes self-care.
– Roll with resistance by engaging the patient in the process of problem solving rather than opposing a patient’s resistance to change behaviors.
– Develop discrepancy by helping the patient recognize that there is an inconsistency between his/her behavior and personal goals.
– Support self-efficacy by empowering the patient to believe that he/she can change behaviors.
6. Demonstrate active listening skills by reflecting and summarizing the patient’s statements. Reflecting and summarizing show the patient that the physician has been listening to concerns and understands what the patient is saying. This is also an opportunity to correct any miscommunications from the visit.
7. Write down instructions or provide handouts to the patient to help reinforce learning and information retention.
8. Ask patients to write a list of questions a few days prior to the medical appointment and bring it with them. Patients are more likely to remember information about issues they have previously considered that directly relate to them.
9. Consider collaborating with community health workers, patient navigators, peer mentors, and other members of the healthcare team to improve communication, diabetes outcomes, and patient satisfaction.
Summary
Physician-patient self-care communication is essential to achieving optimal diabetes outcomes [15,22,33,110] Patients’ ability to inform physicians about their self-care challenges [14], and physicians’ ability to respond to patients’ self-care reports directly and in non-accusatory language, are vital factors in effective diabetes care [45]. Interventions and education that promote open and honest conversations are particularly important given patients’ well-documented struggles achieving self-care and glycemic goals [111] and physicians’ feelings of inadequacy, frustration, and fatigue when they are not making an impact on patients’ outcomes [48,112]. More research is needed to determine the best strategies to improve self-care communication in the physician-patient relationship.
Corresponding author: Elizabeth A. Beverly, PhD, Department of Family Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH 45701, beverle1@ohio.edu.
Financial disclosures: None.
Author contributions: drafting of article, EAB, MFW, ABC, KEP, NNI; critical revision of the article, EAB, MFW, ABC, KEP, NNI.