A Computer-Assisted Process to Reduce Discharge of Emergency Department Patients with Abnormal Vital Signs
Results
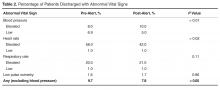
The analysis demonstrated that physicians were, by and large, following recommendations consistent with policies of the American College of Emergency Physicians regarding the management of elevated blood pressures, which do not mandate that patients with asymptomatic elevations of blood pressure receive medical intervention in the ED [12]. In our analysis, the percentage of patients discharged with elevated blood pressures actually increased from 7.5% to 9.9% following the intervention. Importantly, however, the percentage of patients discharged with low blood pressures decreased from 6.9% to 5.0% (P < 0.01).Tthe percent of patients discharged with an elevated heart rate, decreased from 58% in the pre alert group to 42% in the post alert group (P < 0.02).
Discussion
In our study, we used features of the EMR prospectively to affect discharge and then used the database functions of the EMR to assess the effectiveness of those efforts. Previous studies that have looked at the incidence of abnormal vital signs at discharge have been manual, retrospective reviews of records. We are not aware of any studies reporting the results of introducing an EMR alert to prospectively identify patients with abnormal vital signs prior to discharge
While we found that this intervention was successful in reducing clinically relevant abnormal vital signs at discharge, we have realized that the elevated blood pressure alert was unnecessary and we have eliminated it from the programming. We will revisit our strategy to determine if further reducing the high blood pressure alerts can lead to greater improvements in reducing the percentage of patients discharged with abnormal vital signs.
Future plans include a review of the re-visit or hospitalization rate for patients discharged with abnormal vital signs. A companion study evaluating a similar approach to the care of children is under consideration. We are also considering including a field in the EMR for the clinician to document why they discharged a patient with abnormal vital signs.
Corresponding author: Jonathan E. Siff, MD 2500 MetroHealth Drive BG3-65 Cleveland, Ohio 44109 jsiff@metrohealth.org.
Financial disclosures: None.