Comparing risk models guiding growth factor use in chemotherapy
Background The National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) have guidelines for using colony-stimulating factors (CSF) for chemotherapy-induced neutropenia (CIN). Both groups recommend CSF if the chemotherapy has a risk for febrile neutropenia of more than 20%. The guidelines are less definitive if the risk is intermediate (10%-20%). Two risk models developed by Hosmer and Bozcuk and their respective colleagues may provide guidance regarding CSF decision making in this intermediate risk population.
Objective To examine whether risk models developed by Hosmer and Bozcuk had adjunct value to the NCCN and ASCO guidelines when applied to patients with lung cancer who were receiving intermediate-risk chemotherapy.
Methods Male and female patients aged 18-75 years with a diagnosis of any stage lung cancer, small or non-small cell, who required and received their initial chemotherapy at Drexel University in Philadelphia were included in this study. Patients who received growth factor before their chemotherapy were excluded. The Hosmer and Bozcuk calculators for febrile neutropenia risk and the NCCN and ASCO guidelines for using CSF for CIN were applied to this group of patients.
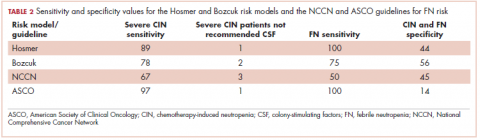
Results 43 patients were included in the study. The Hosmer and Bozcuk calculators and NCCN and ASCO guidelines recommended giving CSF to 26, 22, 25, and 38 patients, respectively. The sensitivities for detecting severe CIN were 89%, 78%, 67%, and 97%, and the specificities were 44%, 56%, 45%, and 14%, respectively.
Limitations Small cohort size; data were limited in scope.
Conclusions In lung cancer patients receiving intermediate-risk chemotherapy, the Hosmer calculator had the best combination of sensitivity, specificity, and ease of use. The NCCN guidelines were less sensitive, whereas the ASCO guidelines were the least specific. Based on these findings, we recommend using the Hosmer calculator because it lends to accurate but judicious use of CSF.
Accepted for publication November 2, 2018
Correspondence Chetan Jeurkar, DO; jeurkar2@gmail.com
Disclosures The authors report no disclosures/conflicts of interest.
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0429
For sensitivity and specificity threshold values, Hosmer reported using a risk score of 10 or above as being a reasonable value for the use of prophylactic CSF. They reported this score would predict an FN risk of about 10%, sensitivity of 24%, and specificity of 93% in detecting FN. 7 Bozcuk reported that using 110 as a cutoff value would correlate to about a 50% FN risk, sensitivity of 100%, and specificity of 49%. However, they did not suggest that value be applied as a threshold for the use of prophylactic CSF as Hosmer did. 8 Despite that, we used the thresholds of 10 and 110 for sensitivity and specificity analyses.
Regarding the current cycle of chemotherapy, the Hosmer calculator looked only at the first cycle, whereas the Bozcuk calculator looked at any cycle of chemotherapy. 7,8 In our study, we used the cycle correlating to the lowest ANC nadir the patient achieved. For example, if a patient achieved a nadir of 1,000 in cycle 1 but 200 in cycle 2, then we used the cycle 2 data to complete the calculators.
With respect to the NCCN and ASCO guidelines, we evaluated our cohort of 43 patients for the risk factors listed in the respective guidelines. If a patient had 1 or more of the risk factors, they were deemed to be high risk and therefore were recommended to receive CSF.
Results
General data
Of the 43 patients studied, 21 developed some level of CIN. Nine patients developed severe CIN, 4 developed moderate CIN, and 8 developed mild CIN. Of the severely neutropenic patients, 4 developed FN. None of the 16 patients who received prophylactic CSF developed FN, although 2 developed severe neutropenia despite CSF administration. Nadirs of ANC were seen on average during cycle 3 of chemotherapy. In all, 15 of the 43 patients achieved lowest ANC nadir during cycle 1.
Risk models
The Bozcuk calculator. A total of 22 patients had risk scores above the calculator’s threshold value of 110. Of those 22 patients, 7 developed severe CIN, 5 developed either mild or moderate CIN, and 3 developed FN. Of the remaining 21 patients who had risk scores of below 110, 2 developed severe CIN, 7 developed mild or moderate CIN, and 1 developed FN. Sensitivity and specificity values are shown in Table 2.
The Hosmer calculator. A total of 26 patients had risk scores above the calculator’s threshold value of 10. Of those 26 patients, 8 developed severe CIN, 4 developed either mild or moderate CIN, and 4 developed FN. Of the remaining 17 patients who had risk scores of less than 10, 1 developed severe CIN, 8 developed mild or moderate CIN, and none developed FN. Sensitivity and specificity values are listed in Table 2.