Symptom burdens related to chemotherapy-induced anemia in stage IV cancer
Background Chemotherapy-induced anemia (CIA) is associated with many symptoms that negatively impact quality of life. However, a systematic examination of symptoms in patients with CIA is lacking.
Objective To describe the occurrence of a comprehensive list of symptoms in patients with stage IV malignancies by CIA status.
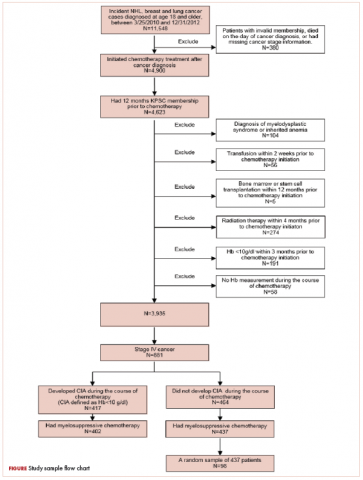
Methods Patients diagnosed with stage IV non-Hodgkin lymphoma, breast, and lung cancer at Kaiser Permanente Southern California (2010-2012) were eligible. CIA was defined as hemoglobin <10 g/dL after the initiation of chemotherapy. Standardized record review evaluated the occurrence of symptoms for all patients who developed CIA (n = 402), and a random sample of patients who did not develop CIA (n = 98). The prevalence of each symptom and the distribution of number of symptoms per patient were described overall and by anemia grade.
Results Mean number of symptoms during chemotherapy for patients who did and did not develop CIA was 6.8 and 4.1, respectively (P < .01). Fatigue (90%), dyspnea or shortness of breath (58%), nausea or vomiting (56%), and loss of appetite (56%) were documented in >50% of patients who developed CIA, whereas only fatigue (77%) was noted in >50% patients without CIA. Several symptoms, including depression, diarrhea, dizziness or lightheadedness, and dyspnea, particularly demonstrated a clearly increasing prevalence with declining hemoglobin level. The mean number of symptoms per patient increased as CIA grade increased (3.6 symptoms for grade 2, and 5.4 symptoms for grades 3 and 4, respectively).
Limitations No causal relationship was examined due to descriptive design.
Conclusions High-grade CIA correlates with an increased symptom burden in patients with stage IV malignancies.
Funding Amgen Inc, maker of ESA used in the treatment of anemia
Accepted for publication October 26, 2018
Correspondence Chun Chao, PhD; Chun.R.Chao@kp.org
Disclosures Hairong Xu and Bhakti Mehta were employees of Amgen during study execution and received salary and stock as part of employment. Amgen provided research support to Kaiser Permanente to perform this study who, in turn, employed or contracted with the non-Amgen authors. Authors did not report any other potential conflicts of interest.
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0432
Results
A total of 402 stage IV NHL, breast, and lung cancer patients who developed CIA and 98 patients who did not develop CIA during the first course of chemotherapy were included (Figure 1).
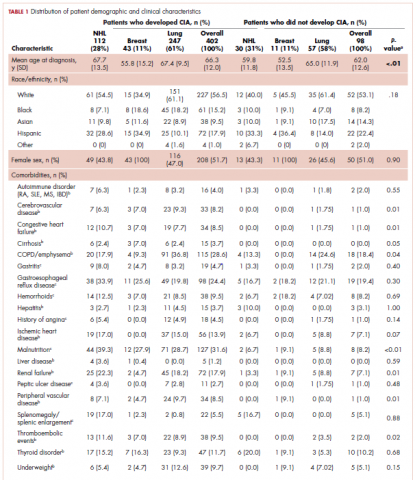
The distribution of cancer types in the study sample were similar across CIA status (Table 1). The mean age at diagnosis was 66 years in patients who developed CIA and 62 years in patients who did not develop CIA. Women accounted for half of the patients in both study samples (52% and 51%, respectively). Most of the study patients were of non-Hispanic white race/ethnicity. Chronic obstructive pulmonary disease/emphysema and gastroesophageal reflux disease were among the most common comorbidities examined in both study samples, while malnutrition and moderate to severe renal disease were also common in patients who developed CIA (Table 1).
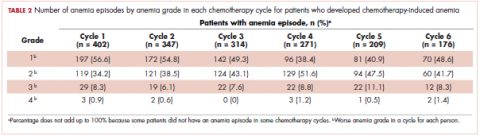
,The mean Hb level before chemotherapy was lower for patients who developed CIA compared with patients who did not develop CIA (12.3 g/dL and 13.5 g/dL, respectively; Table 1). The mean lowest Hb level during chemotherapy was 8.5 g/dL for patients who developed CIA and 11.4 g/dL for patients without CIA (Table 1). The number of anemia events by grade in each chemotherapy cycle in patients who developed CIA is shown in Table 2.
Table 3 shows the number and proportion of study patients with each of the symptoms documented before and after chemotherapy initiation for the 2 study samples. Patients who developed CIA had statistically significantly more pre-existing symptoms, incident symptoms, or any symptoms that occurred during chemotherapy compared with patients who did not develop CIA.
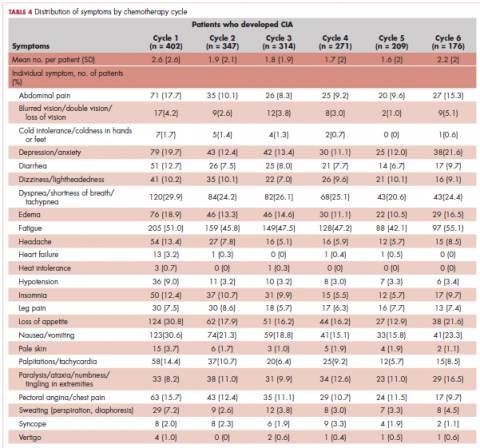
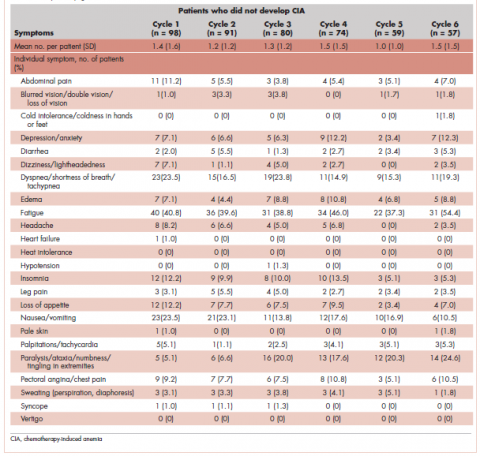
Table 4 shows the number and proportion of study patients with symptoms that occurred during each chemotherapy cycle. Again, fatigue is the predominant symptom documented throughout cycles for all patients. In patients who developed CIA, the proportion of patients experiencing the following symptoms was relatively stable across chemotherapy cycles: depression/anxiety, dizziness/lightheadedness, fatigue, pale skin, and sweating. The proportion of patients experiencing paralysis/ataxia/numbness/tingling in extremities increased over cycles. For headache, loss of appetite, hypotension, and nausea/vomiting, the proportion of patients with symptom documentation was highest in cycle 1, stabilizing in subsequent cycles (Table 4). In patients without CIA, the cycle-level prevalence of most of the symptoms did not increase over cycles, except for paralysis/ataxia/numbness or tingling in extremities. For insomnia, loss of appetite, and nausea/vomiting, the cycle-level prevalence dropped after the first cycle. There was no clear increasing trend of the mean number of symptoms per patient across chemotherapy cycles in both study samples (Table 4).
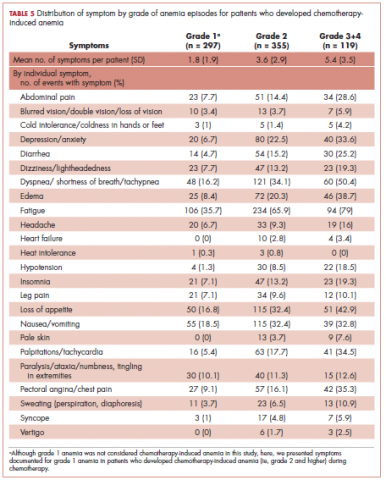
Table 5 shows the distribution of symptoms by anemia grade in patients who developed CIA. In general, the prevalence of symptoms increased with higher grades of anemia. The following symptoms especially have a clear increase in prevalence as the severity of anemia progressed: abdominal pain, depression, diarrhea, dizziness/lightheadedness, dyspnea, edema, fatigue, heart failure, headache, hypotension, insomnia, leg pain, loss of appetite, pale skin, palpitations, pectoral angina, and sweating. The mean number of symptoms per patient increased as CIA grade increased, from 3.6 (SD, 2.9) for grade 2 CIA to 5.4 (SD, 3.5) for grades 3 and 4 CIA (specifically, 5.3 [SD, 3.4] for grade 3 CIA and 6.4 [SD, 4.1] for grade 4 CIA; data not shown) (Table 5).
When stratified by gender, there are no material differences between men and women in most analyses. In men, the mean number of pre-existing symptoms was 1.7 (SD, 1.8) and 1.0 (SD, 1.2) for those with and without CIA, respectively (P = .02). The mean number of symptoms that occurred during chemotherapy was 7.0 (SD, 3.4) and 4.2 (SD, 2.4), respectively (P < .01). In women, the mean number of pre-existing symptoms was not statistically different in those with and without CIA (1.6 [SD, 2.2] and 1.3 [SD, 1.8], respectively; P = .46). However, like in men, the mean number of symptoms that occurred during chemotherapy was significantly more in those with CIA (6.5 [SD, 3.3] and 4.0 [SD, 2.9], respectively; P < .01). As in the overall analysis, there was no clear increasing trend of the number of symptoms per patients across chemotherapy cycles in both men and women, but the average number of symptoms increased as the CIA grade increased. For men, the mean number of symptoms per patient increased from 3.7 (SD, 3.0) for grade 2 CIA to 6.0 (SD, 3.5) for grades 3 and 4 CIA (data not shown). For women, the mean number of symptoms per patient increased from 3.6 (SD, 2.9) for grade 2 CIA to 4.7 (SD, 3.3) for grades 3 and 4 CIA (data not shown).