The long-term effects of posttreatment exercise on pain in young women with breast cancer

Background Persistent pain after treatment has been identified in breast cancer populations, with prevalence rates ranging from 25%-60%. Age, surgical procedure, axillary node dissection, and radiation therapy have shown correlation with chronic pain development.
Objective To conduct a pilot randomized controlled trial targeting young breast cancer patients to determine the effectiveness of a 12-week exercise program on long-term levels of upper-limb pain, as measured by the Brief Pain Inventory-Short Form (BPI-SF), and pain measured by physical examination of specific shoulder movements.
Methods Young adults (18-45 years of age) recently diagnosed with breast cancer consenting to participate in this study were randomly allocated to intervention or control groups. The exercise intervention group participated in a 12-week exercise program starting 3-4 weeks after the cessation of radiation therapy, and the control group received standard care consisting of encouragement for an active lifestyle and pamphlets on the benefits of exercise. The location and severity of pain and its interference with daily life were recorded at the following 6 time points: postsurgery and preradiation (T1, baseline), postradiation and preintervention (T2), and 4 points during an 18-month period postradiation (T3-T6 at 3, 6, 12, and 18 months). In addition, clinical physical assessment of range of motion and pain on active shoulder movements were recorded at each time point.
Results 59 young breast cancer patients participated in the study (exercise group: n = 29; control group: n = 30). Over the course of the trial, there were no significant differences between study groups in the BPI-SF measures of pain interference and severity scores. Improvements in pain on shoulder movements were noted in the intervention group at 3 and 6 months postintervention (T3 and T4) but were not sustained over time (by T6, 18 months postradiation). Shoulder girdle-chest wall pain improved at 12 and 18 months postradiation in both groups but persisted despite exercise intervention. Recordings of shoulder pain on physical examination of range showed a distinct pattern of temporal improvement (T3-T5), followed by low levels of pain recurrence at 18 months postradiation (T6) in both groups.
Limitations Stringent exclusion criteria, including the absence of any shoulder pathology or pre-existent medical comorbidities impacting upper limb function, long-term follow-up, and the relatively small population of breast cancer patients in this age demographic, limited and prolonged recruitment for this study. In addition, the general activity levels of the young breast cancer survivors who agreed to participate in this exercise intervention study may have had an impact on the significance of results.
Conclusion Transient improvements in shoulder pain can be attributed to a 12-week exercise program, but they did not translate to long-term benefits. Moreover, the BPI-SF did not capture shoulder pain and limitations related to upper-limb disability in this study, in contrast with the findings on physical examination.
Funding This study was funded by Hope & Cope, a grant from the CURE Foundation, and grants from the Jewish General Hospital's Weekend to End Breast Cancer.
Accepted for publication May 15, 2018
Correspondence Mary-Ann Dalzell, MScxPT; madalzell5@gmail.com
Disclosures Thierry Muanza holds an intellectual property patent (United States Provisional Patent Application No. 62/359,918; Title: Adipose Mesenchymal Stromal Cells for Treating Radiation-Induced Oral Mucositis). Mary-Ann Dalzell, Richard Dalfen, Beatrice Fournier, Marize Ibrahim, Petr Kavan, Michael Palumbo, Warren Sateren, and Nadia Smirnow report no disclosures or conflicts of interest.
Citation JCSO 2018;16(3):e145-e151
©2018 Frontline Medical Communications
doi https://doi.org/10.12788/jcso.0395
Related articles
Measurement of physical activity and sedentary behavior in breast cancer survivors
Effects of exercise interventions during different treatments in breast cancer
Submit a paper here
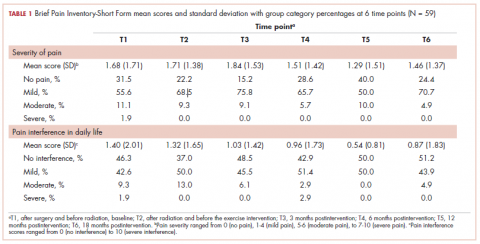
The findings showed that there was little variance between the intervention and control groups in BPI-SF severity scores from T1 to T6, so the means and SDs of the BPI-SF scores were grouped at 6 time points (Table 1). There was no statistically significant difference between baseline measures at T1 (1.68; SD, 1.17) and measures at 18 months postintervention (T6: 1.46; SD, 1.37). At baseline, 87.7% of the women reported no pain (31.5%) or mild levels of pain (55.6%), and 13% reported moderate or severe pain. Over the duration of the study from T1 to T6, these primarily low levels of pain (BPI-SF, 0-4) remained consistent with a favorable shift toward having no pain (T1: 31.5%; T6: 24.4%). By 18 months postintervention, 95.7% of women reported no or mild pain, with 4.9% reporting moderate pain.
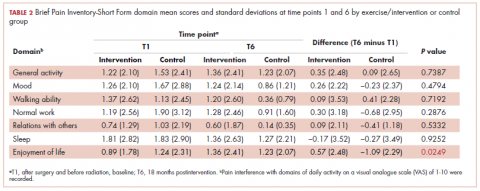
Similarly, there was little variance over time (T1-T6) and no statistically significant differences between the 2 groups in BPI-SF–measured levels of pain interference in daily activities (Table 2). Moreover, a domain analysis showed that there were no statistically significant differences in pain interference scores when comparing the type and extent of surgery (total mastectomy: 0.59 [1.17]; lumpectomy: 0.94 [1.96]). By chance – and not related directly to the objectives of this study – there was a statistically significant difference between the intervention and control groups in the interference of pain on the Enjoyment of Life domain in favor of the control group.
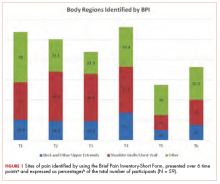
The sites of pain captured by the BPI-SF shed light on the preceding findings (Figure 1). At baseline (T1, postsurgery and preradiation), 37.0% of participants reported pain in the shoulder girdle–chest wall region, whereas 20.4% reported pain in the general neck–upper extremity region and 50% in other regions. Postradiation, shoulder girdle–chest wall pain was identified as the highest reported site of pain (49.1%; T2, postradiation and preintervention) and remained elevated at 3 months (T3) and 6 months (T4) postradiation (46.9% and 45.5%, respectively). At 12 and 18 months postradiation (T5 and T6), the principal focus of pain shifted once again to “other” regions at 30% and 32.5%, respectively, and the neck–upper extremity region at 10% and 15%, respectively. Shoulder girdle–chest wall pain concomitantly improved at those time points (15% and 25% respectively) but was not eliminated.
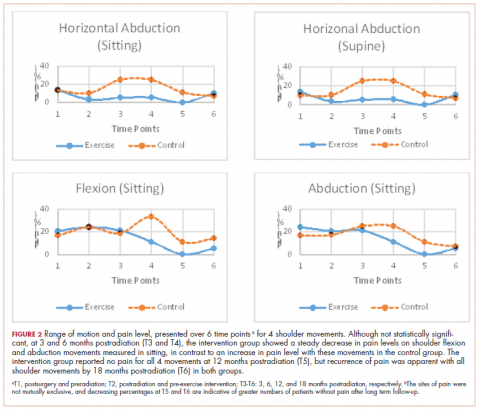
Pain levels recorded on physical examination for isolated shoulder range of movements were recently published,24 and they have been abbreviated and reproduced in this paper (Figure 2) to allow for a comparison of findings between the exercise intervention group and the control group to help determine the sensitivity of these tools for use in breast cancer patients. At baseline, pain levels with active movement were noted to be slightly greater in the intervention group for flexion and abduction.
Following the intervention, at 3 and 6 months postradiation (T3 and T4), the intervention group showed a steady decrease in pain levels in flexion and abduction, whereas the control group showed a 5-fold increase in pain with horizontal abduction. Furthermore, participants in the intervention group reported having no pain on movement 12 months postradiation (T5); however, recurrence of pain was apparent with all shoulder movements by 18 months postradiation (T6) in both the intervention and control groups.
Discussion
Previous studies have hypothesized that younger age (18-39 years), adjuvant radiotherapy, and axillary node dissection are risk factors for chronic pain in breast cancer survivors.22,25 Persistent pain is prevalent in 12% to 51% of breast cancer survivors, with up to one-third experiencing some pain more than 5 years after treatment,26,27 and our study outcomes concur with those findings. In our study, pain, as measured by the BPI-SF, was found to persist for most participants (75.6%) after the 18-month follow-up. The results of our trial showed that a 12-week exercise intervention administered postsurgery and postradiation had no statistically significant effect on long-term (18 months) pain severity and its interference in daily life. It is worth noting that body regions that had not been directly related to either surgical or radiation treatment for breast cancer were commonly identified as areas of pain but were not specifically targeted by our intervention. However, focusing on pain severity (BPI-SF), our findings suggest that the benefits of targeted upper-extremity exercise on pain in the intermediate time course of follow-up (T3, T4, and T5) was notable compared with the control group, which received standard care. The apparent recurrence of pain at 18 months in both groups was not anticipated and needs to be further investigated.