Advanced training options in inflammatory bowel disease
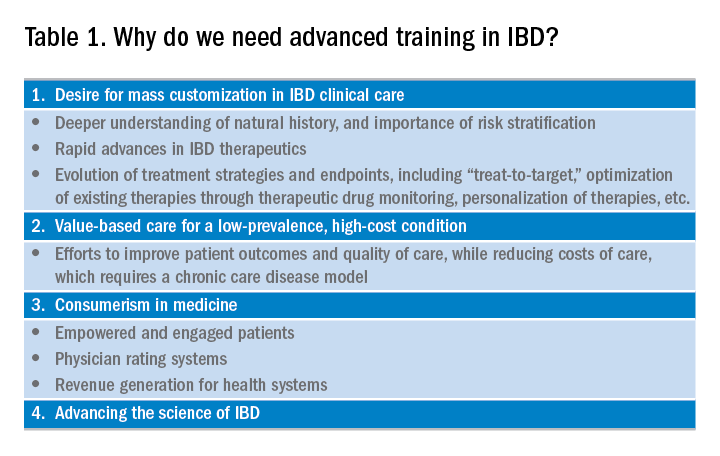
The global incidence and prevalence of inflammatory bowel disease (IBD) is rising, and it is estimated that by 2025, approximately 2.2 million Americans will be living with this disease. At the same time, there have been several paradigm-changing scientific and medical advances in the understanding and management of IBD. As the diagnostic, therapeutic, and monitoring armamentarium in the management of IBD increases, so is the complexity of the decision making. Advanced concepts and training are often not covered adequately during a general gastroenterology fellowship. In a survey of 160 trainees, more than one-third of fellows did not feel “confident” or “mostly comfortable” with their level of IBD training. Yet, efficient dissemination, effective translation and integration of these advances into clinical practice is paramount to improving quality of care. To facilitate multiple goals as listed in Table 1, advanced training in the field of IBD is increasingly important. In this article, I review different training options available for young gastroenterologists.
Readers are also directed to an excellent article by David Rubin, MD, published in Gastroenterology in 2015.
Advanced fellowship training in IBD
The most rigorous training in IBD is offered through dedicated advanced fellowships. Currently, there are more than 20 such fellowships in North America, most of them offered at large academic centers with nationally and internationally renowned faculty. These training positions are generally 1 year long, offered after completion of gastroenterology fellowship. The Accreditation Council of the Graduate Medical Education (ACGME) does not accredit these advanced training programs, and there is not a separate American Board of Internal Medicine (ABIM) certification for IBD. Funding of such programs comes from different sources including endowments, private foundations, institutional funds, pharmaceutical company grants, and even limited faculty appointments of the trainees. Though there is currently no official regulatory oversight and requirements, most programs have well-defined curricula covering diverse aspects of IBD care. This core curriculum has been nicely summarized in a recent article by Uma Mahadevan, MD, in Gastroenterology.
Clinical training in these programs is offered through a mix of outpatient IBD clinics (generally three to five clinics/week, with one or more senior IBD-focused faculty member), supervising general gastroenterology fellows for inpatient IBD care, dedicated IBD-focused endoscopy sessions (generally one or two sessions/week) including chromoendoscopy and stricture dilation, as well as formal and informal mentorship by one or more senior faculty members, time and mentorship for scholarly activities, and appropriate evaluation and feedback systems. In addition, most programs offer multidisciplinary training through dedicated clinics with colorectal surgeons (such as pouch clinics, etc.), opportunities for observing and interacting with radiologists, pathologists, psychologists, and dietitians.







