Effect of Multidisciplinary Transitional Pain Service on Health Care Use and Costs Following Orthopedic Surgery
Background: Opioid use disorder is a significant cause of morbidity, mortality, and health care costs. A transitional pain service (TPS) approach to perioperative pain management has been shown to reduce opioid use among patients undergoing orthopedic joint surgery. However, whether TPS also leads to lower health care use and costs is unknown.
Methods: We designed this study to estimate the effect of TPS implementation relative to standard care on health care use and associated costs of care following orthopedic surgery. We evaluated postoperative health care use and costs for patients who underwent orthopedic joint surgery at 6 US Department of Veterans Affairs medical centers (VAMCs) between 2018 and 2019 using difference-in-differences analysis. Patients enrolled in the TPS at the Salt Lake City VAMC were matched to control patients undergoing the same surgeries at 5 different VAMCs without a TPS. We stratified patients based on history of preoperative opioid use into chronic opioid use (COU) and nonopioid use (NOU) groups and analyzed them separately.
Results: For NOU patients, TPS was associated with a mean increase in the number of outpatient visits (6.9 visits; P < .001), no change in outpatient costs, and a mean decrease in inpatient costs (−$12,170; P = .02) during the 1-year follow-up period. TPS was not found to increase health care use or costs for COU patients.
Conclusions: Although TPS led to an increase in outpatient visits for NOU patients, there was no increase in outpatient costs and a decrease in inpatient costs after orthopedic surgery. Further, there was no added cost for managing COU patients with a TPS. These findings suggest that TPS can be implemented to reduce opioid use following joint surgery without increasing health care costs.
RESULTS
Of the 4954 patients included in our study cohort, 3545 (71.6%) were in the NOU group and 1409 (28.4%) were in the COU group. Among the NOU cohort, 361 patients were in the intervention group and 3184 in the control group. Among the COU cohort, 149 patients were in the intervention group and 1260 in the control group (Table 1). Most patients were male, White race, with a mean (SD) age of 64 (11) years. The most common orthopedic procedure was total knee arthroplasty, followed by total hip arthroplasty. Among both NOU and COU cohorts, patients’ characteristics were similar between the pre- and postintervention period among either TPS or control cohort.
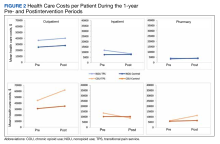
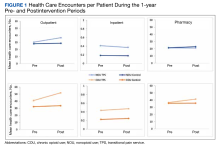
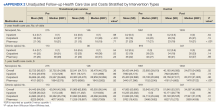
Figures 1 and 2 and eAppendix 2 depict unadjusted per-person average outpatient, inpatient, and pharmacy visits and costs incurred during the 1-year pre- and postintervention periods for the NOU and COU cohorts. Average total health care follow-up costs ranged from $40,000 to $53,000 for NOU and from $47,000 to $82,000 for COU cohort. Cost for outpatient visits accounted for about 70% of the average total costs, followed by costs for inpatient visits of about 20%, and costs for pharmacy for the remaining.
For the NOU cohort, the number of health care encounters remained fairly stable between periods except for the outpatient visits among the TPS group. The TPS group experienced an increase in mean outpatient visits in the postperiod: 30 vs 37 visits (23%) (
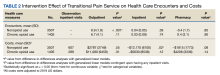
Table 2 summarizes the results from the multivariable DID analyses for the outpatient, inpatient, and pharmacy visit and cost outcomes. Here, the estimated effect of the TPS intervention is the coefficient from the interaction between the postintervention and TPS exposure indicator variables. This coefficient was calculated as the difference in the outcome before and after the TPS intervention among the TPS group minus the difference in the outcome before and after the TPS intervention among the control group. For the NOU cohort, TPS was associated with an increase in the use of outpatient health care (mean [SD] increase of 6.9 [2] visits; P < .001) after the surgery with no statistically significant effect on outpatient costs (mean [SD] increase of $2787 [$3749]; P = .55). There was no statistically significant effect of TPS on the use of inpatient visits or pharmacy, but a decrease in costs for inpatient visits among those who had at least 1 inpatient visit (mean [SD] decrease of $12,170 [$6100]; P = .02). For the COU cohort, TPS had no statistically significant impact on the use of outpatient, inpatient, or pharmacy or the corresponding costs.