Lumbar Fusion With Polyetheretherketone Rods Use for Patients With Degenerative Disease
Introduction: Polyetheretherketone (PEEK) rods for lumbar fusion have been available since 2007. However, literature about their utility is sparse and of mixed outcomes.
Methods: A retrospective review of PEEK rod lumbar fusion cases was performed. Data were analyzed from 108 patients of the senior author Donald Ross who underwent PEEK lumbar fusion.
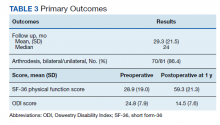
Results: There were 97 single and 11 2-level fusions. Rates of tobacco use, diabetes mellitus, low bone density, depression, and immunosuppression were 23.1%, 24.1%, 14.8%, 32.4%, and 6.5%, respectively. In the study population, the mean age was 60.2 years, body mass index was 30.1, and there was a mean 31.3 months for follow-up. There were no wound infections or new neurologic deficits. Of 81 patients with > 11 months of follow-up, 70 (86.4%) had an arthrodesis, 8 (9.9%) had no ar throdesis, and 3 (3.7%) were indeterminate. No patients had revision fusion surgery and 2 patients had adjacent level fusions at 27 and 60 months. One patient had an adjacent segment laminectomy at 18 months and one a foraminotomy at 89 months, resulting in a 3.7% adjacent segment surgery rate. Mean preoperative Short Form-36 (SF-36) physical functioning (PF) score and Oswestry Disability Index (ODI) score were 28.9 and 24.8, respectively. Mean SF-36 PF postoperative score at 1 and 2 years were 59.3 and 65, respectively. Mean ODI postoperative score at 1 year was 14.5.
Conclusions: In a large patient cohort lumbar fusion with PEEK rods can be undertaken with low complication rates, satisfactory clinical improvements, low rates of hardware failure or need for revision surgery. Longer follow-up is needed to confirm findings.
Imaging
Final imaging was by radiograph in 73 patients, CT in 31, and magnetic resonance imaging (MRI) in 3 (1 patient had no imaging). Sixty-seven patients (62.0%) had a bilateral arthrodesis, and 15 (13.9%) had at least a unilateral arthrodesis. MRI was not used to assess arthrodesis. Eight patients (7.4%) had no definite arthrodesis. Seventeen patients had inadequate or early imaging from which a fusion determination could not be made. Of 81 patients with > 11 months of follow up, 58 (71.6%) had a bilateral arthrodesis, 12 (14.8%) had a unilateral arthrodesis, 8 (9.9%) had no arthrodesis, and 3 (3.7%) were indeterminate.
No patient had any revision fusion surgery at the index level during follow up. Two patients had adjacent level fusions at 27 and 60 months after the index procedure. One patient had a laminectomy at an adjacent segment at 18 months postfusion, and 1 had a foraminotomy at an adjacent segment 89 months post fusion (Figure 3). Overall, there were 4 (3.7%) adjacent segment surgeries at a mean of 48.5 months after surgery. One patient had a sacro-iliac joint fusion below an L5-S1 fusion 17 months prior for persisting pain after the fusion procedure.
Patient Reported Outcomes
Preoperative SF-36 PF and ODI scores were available for 81 patients (Table 3). Postoperative SF-36 PF scores were obtained at 3 months for 65 of these patients, and at 1 year for 63 patients. Postoperative ODI scores were obtained at 3 months for 65 patients, and at 1 year for 55 patients. Among the 65 patients with completed SF-36 scores at 3 months, a mean increase of 22.4 (95% CI, 17-27; P < .001) was noted, and for the 63 patients at 1 year a mean increase of 30.3 (95% CI, 25-35; P < .001) was noted. Among the 65 patients with completed ODI scores at 3 months, a mean decrease of 6.8 (95% CI, 4.9-8.6; P < .001) was noted, and for the 55 patients with completed ODI scores at 1 year a mean decrease of 10.3 (n = 55; 95% CI, 8.4-12.2; P < .001) was noted.
Cost
We compared the hardware cost of a single level construct consisting of 4 pedicle screws, 4 locking caps, and 2 rods using a PEEK system with that of 2 other titanium construct systems. At VAPHCS, the PEEK system cost was about 71% of the cost of 2 other titanium construct systems and 62% of the cost when compared with Medtronic titanium rods.
Discussion
PEEK is useful for spine and cranial implants. It is inert and fully biocompatible with a modulus of elasticity between that of cortical and cancellous bone, and much lower than that of titanium, and is therefore considered to be semirigid.3,4,6 PEEK rods are intermediate in stiffness between titanium rods (110 Gigapascals) and dynamic devices such as the Zimmer Biomet DYNESYS dynamic stabilization system or the Premia Spine TOPS system.3 Carbon fiber rods and carbon fiber reinforced PEEK implants are other semirigid rod alternatives.7,8 PEEK rods for posterior lumbar fusion surgery were introduced in 2007. Li and colleagues provide a thorough review of the biomechanical properties of PEEK rods.3