Lumbar Fusion With Polyetheretherketone Rods Use for Patients With Degenerative Disease
Introduction: Polyetheretherketone (PEEK) rods for lumbar fusion have been available since 2007. However, literature about their utility is sparse and of mixed outcomes.
Methods: A retrospective review of PEEK rod lumbar fusion cases was performed. Data were analyzed from 108 patients of the senior author Donald Ross who underwent PEEK lumbar fusion.
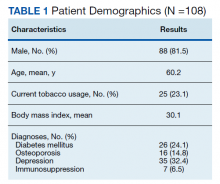
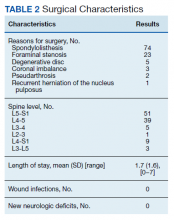
Results: There were 97 single and 11 2-level fusions. Rates of tobacco use, diabetes mellitus, low bone density, depression, and immunosuppression were 23.1%, 24.1%, 14.8%, 32.4%, and 6.5%, respectively. In the study population, the mean age was 60.2 years, body mass index was 30.1, and there was a mean 31.3 months for follow-up. There were no wound infections or new neurologic deficits. Of 81 patients with > 11 months of follow-up, 70 (86.4%) had an arthrodesis, 8 (9.9%) had no ar throdesis, and 3 (3.7%) were indeterminate. No patients had revision fusion surgery and 2 patients had adjacent level fusions at 27 and 60 months. One patient had an adjacent segment laminectomy at 18 months and one a foraminotomy at 89 months, resulting in a 3.7% adjacent segment surgery rate. Mean preoperative Short Form-36 (SF-36) physical functioning (PF) score and Oswestry Disability Index (ODI) score were 28.9 and 24.8, respectively. Mean SF-36 PF postoperative score at 1 and 2 years were 59.3 and 65, respectively. Mean ODI postoperative score at 1 year was 14.5.
Conclusions: In a large patient cohort lumbar fusion with PEEK rods can be undertaken with low complication rates, satisfactory clinical improvements, low rates of hardware failure or need for revision surgery. Longer follow-up is needed to confirm findings.
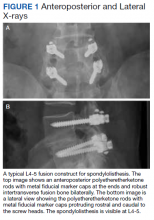
Surgeries were conducted on a Mizuho OSI Jackson Table via bilateral 3 to 4 cm Wiltse incisions using the Medtronic Quadrant retractor system. Medtronic O-Arm images were acquired and delivered to a Medtronic Stealth Station for navigation of the screws. Monopolar coagulation was not used. PEEK pedicle screws were placed and verified with a second O-Arm spin before placing lordotic PEEK rods in the screw heads. No attempt was made to reduce any spondylolisthesis, but distraction was used to open the foramina and indirectly decompress the canal. An interbody device was placed only in treatment of multiply recurrent disc protrusion. After decortication of the transverse processes and facets, intertransverse fusion constructs consisting of calcium hydroxyapatite soaked in autologous bone marrow blood and wrapped in 6-mg bone morphogenetic protein-soaked sponges were placed on the bone. If canal decompression was indicated, a Medtronic Metrx retractor tube was then placed through one of the incisions and decompression carried out. Wounds were closed with absorbable suture. No bracing was used postoperatively. Figure 1 shows a typical single level PEEK rod fusion construct.
Patient pre- and postoperative Short Form-36 (SF-36) physical function (PF) scores and Oswestry Disability Index (ODI) scores had been obtained at routine clinic visits.
Static radiographs were used to assess the fusion. Dynamic films and/or computed tomography (CT) scans were obtained only when symptomatic pseudarthrosis was suspected. Some patients had abdominal or lumbar CT scans for other indications, and these were reviewed when available. Particular care was taken to assess facet fusion as an indicator of arthrodesis (Figure 2).5
Statistical Analysis
Pre- and postoperative pairwise t tests were completed for patients with a complete data, using SAS 9.2 statistical package. Data are presented as standard deviation (SD) of the mean.
Results
Following application of the inclusion/exclusion criteria, 108 patients had undergone lumbar fusion with PEEK rods. Mean (SD) patient age was 60.2 (10.3) years and 88 patients were male (Table 1). Most surgeries were at L5-S1 and L4-5. There were 97 single-level fusions and 11 bilevel fusions. Seventy-four procedures were for spondylolisthesis, 23 for foraminal stenosis, 5 for degenerative disc disease, 3 for coronal imbalance with foraminal stenosis, 2 for pseudarthrosis after surgery elsewhere, and 1 for multiple recurrent disc herniation (Table 2). Twenty-five patients (23.1%) were current tobacco users and 28 (25.9%) were former smokers, 26 (24.1%) had diabetes mellitus (DM), 16 (14.8%) had low bone density by dual energy X-ray absorptiometry (DEXA) imaging, 35 (32.4%) had depression, and 7 (6.5%) were taking an immunosuppressive agent (chronic steroids, biological response modifiers, or methotrexate). Mean body mass index was 30.1.
Surgical Procedure
Of the 108 patients, the first 18 underwent a procedure with fluoroscopic guidance and the Medtronic FluoroNav and Stealth Systems. The next 90 patients underwent a procedure with O-Arm intraoperative CT scanning and Stealth frameless stereotactic navigation. The mean (SD) length of stay was 1.7 (1.3) days. There were no wound infections and no new neurologic deficits. Mean (SD) follow up time was 30.3 (21.8) months.