Biofeedback in headache: An overview of approaches and evidence
ABSTRACT
Biofeedback-related approaches to headache therapy fall into two broad categories: general biofeedback techniques (often augmented by relaxation-based strategies) and methods linked more directly to the pathophysiology underlying headache. The use of general biofeedback-assisted relaxation techniques for headache has been evaluated extensively by expert panels and meta-analyses. Taken together, these reviews indicate that (1) various forms of biofeedback are effective for migraine and tension-type headache; (2) outcomes with biofeedback rival outcomes with medication therapy; (3) combining biofeedback with medication can enhance outcomes; and (4) despite efficacy in many patients, biofeedback fails to bring significant relief to a sizeable number of headache patients. Biofeedback methods that more directly target headache pathophysiology have focused chiefly on migraine. These headache-specific approaches include blood volume pulse biofeedback, which has considerable supportive evidence, and electroencephalographic feedback.
Interim conclusions
Consideration of the findings from individual studies and reviews discussed, plus those not singled out here, leads to the following conclusions:
1) Various forms of biofeedback are effective for migraine and tension-type headache.
2) Outcomes with these forms of biofeedback rival outcomes with medication alone.
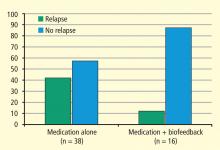
3) Combining biofeedback with medication can enhance outcomes.
4) Outcomes from biofeedback are similar to those obtained with other behavioral approaches. Whether biofeedback has a unique advantage over other similar approaches is not known, but at least one investigation suggests that biofeedback may be of particular value to a subset of patients.14
5) Although not reviewed here, the outcome effects from biofeedback seem to endure for extended periods,15 whether booster treatments are provided or not.16
6) Although biofeedback has been shown to be effective for a number of patients, a sizeable number of patients do not achieve significant relief.
Remaining questions and challenges
Unfortunately, little attention has been devoted to identifying variables predictive of outcome. Certain headache types—chronic forms of headache (presence of pain ≥ 15 days per month), headaches associated with the menstrual cycle, headaches accompanied by medication overuse (of ergotamine, triptans, analgesics, or opioids), posttraumatic headaches, and cluster headaches—have shown minimal response to biofeedback alone.
EVIDENCE BASE FOR HEADACHE-SPECIFIC BIOFEEDBACK APPROACHES
As noted above, a number of biofeedback approaches have been suggested that are tied more directly to the underlying physiology of headache.
Blood volume pulse biofeedback
One of these approaches, blood volume pulse (BVP) biofeedback, has undergone a sufficient number of trials to be included in the recent meta-analysis by Nestoriuc et al8 mentioned earlier. This approach involves monitoring blood flow in the temporal artery and providing feedback to patients to enable them to decrease or constrict blood flow. This approach, when first envisioned,18 was viewed as the nondrug counterpart to the abortive agent ergotamine. Although BVP biofeedback is not very common in clinical practice, the meta-analysis by Nestoriuc et al8 found it to produce the greatest effect size of the biofeedback methods assessed for migraine relief (Figure 1).