Autonomic function and prognosis
ABSTRACT
Autonomic nervous system function is assessed in the clinic by measuring resting heart rate, heart rate variability, or heart rate recovery following exercise. Each of these measures is a strong predictor of cardiovascular risk and all-cause mortality in primary and secondary prevention settings. These measures have been used to identify correlates of autonomic nervous system dysfunction at both the patient level (eg, obesity, diabetes, heart failure) and the environmental level (eg, smoking, social stress, air pollution). Future research must determine how to exploit the associations between autonomic system dysfunction and poor prognosis to improve patient outcomes.
Heart rate recovery
In 1999, Cole and colleagues reported on the association between heart rate recovery during the first minute after exercise and all-cause mortality in approximately 2,400 patients who were candidates for first-time coronary angiography.6 An abnormal heart rate recovery was defined as a reduction from the peak heart rate of 12 beats per minute or less, which corresponded to the lowest quartile. Thus, a patient achieving a peak heart rate of 160 beats per minute would be considered to have an abnormal heart rate recovery if 1 minute later the heart rate was 148 beats per minute or higher. Patients who had an abnormal heart rate recovery had a nearly fourfold increased risk of all-cause death; even after adjusting for numerous confounders, including exercise capacity, there was still a twofold independent increased risk of death. This initial observation has since been confirmed in other cohorts.19,20 The link between heart rate recovery, mortality, and cardiovascular prognosis appears to be independent of symptom status,21 type of recovery protocol,22 left ventricular ejection fraction,22 and angiographic severity of coronary artery disease.23
The mechanism by which an abnormal heart rate recovery predicts increased mortality is unclear. Given that heart rate recovery is thought to reflect parasympathetic nervous system function, and given that increased parasympathetic tone is believed to have antiarrhythmic effects, one might hypothesize that lower heart rate recovery would predict sudden cardiac death. In 2005, investigators from the Paris Civil Service Study reported on the association of exercise heart rate recovery and type of mortality; low heart rate recovery was strongly predictive of sudden cardiac death but not of non-sudden cardiac myocardial infarction death.20 A separate study from the Cleveland Clinic showed that among more than 29,000 patients, frequent ventricular ectopy during early recovery was strongly predictive of death, whereas frequent ventricular ectopy during exercise was not.24 These two studies together suggest that the link between heart rate recovery and mortality may be a reflection of the antiarrhythmic properties of the parasympathetic nervous system.
It is well known that there is an exceptionally powerful link between functional capacity and cardiovascular risk.25,26 People who are in excellent physical shape have high levels of parasympathetic tone. Among patients with suspected coronary artery disease, there is a strong dose-response relationship between heart rate recovery and physical fitness.6 While the link between functional capacity and prognosis is complex, it is conceivable that parasympathetic protection against arrhythmias and shear-induced plaque rupture may play a role.
DETERMINANTS OF AUTONOMIC NERVOUS SYSTEM FUNCTION
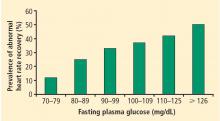
There is an extensive literature documenting a number of determinants of autonomic tone.3,7 On a patient level, decreased levels of parasympathetic tone or increased levels of sympathetic tone have been linked to obesity, insulin resistance, diabetes, hypertension, hypercholesterolemia, depression, anxiety, heart failure, and peripheral vascular disease.3
Perturbations of autonomic nervous system function have also been associated with environmental exposures. People who have lower levels of education,29 live in neighborhoods characterized by lower socio-economic status,30 or are exposed to small-particulate air pollution31 have been shown to manifest abnormal heart rate recovery or decreased heart rate variability.
CONCLUSIONS
Autonomic nervous system function can be measured in the clinic by recording resting heart rate, heart rate variability, or exercise heart rate recovery.1 All three of these measures are strong predictors of cardiovascular risk and all-cause mortality in both primary and secondary prevention settings. A number of determinants of autonomic nervous system function have been identified, including patient-level factors like obesity, diabetes, and heart failure as well as environmental correlates like smoking, social stress, and air pollution. It is not yet known, however, how best to take advantage of the associations between abnormal autonomic nervous system function and poor prognosis to improve patient outcomes. Future research will be needed to identify strategies of favorably modulating autonomic function that improve outcomes in the clinic and among large populations.