An overview of venous thromboembolism: Impact, risks, and issues in prophylaxis
ABSTRACTVenous thromboembolism (VTE) is a major cause of cardiovascular death, and its close association with increased age portends an increasing clinical and economic impact for VTE as the US population ages. Studies show that rates of VTE prophylaxis remain inadequate both in the hospital and at the time of discharge. Health care accreditation and quality organizations are taking interest in VTE risk assessment and prophylaxis as a measure for hospital performance ratings and even reimbursement. To set the stage for the rest of this supplement, this article reviews the rationale for VTE prophylaxis, surveys current prophylaxis rates and strategies to increase those rates, and provides an overview of risk factors for VTE and therapeutic options for VTE prophylaxis.
Venous thromboembolism (VTE)—which comprises both deep vein thrombosis (DVT) and pulmonary embolism (PE), which can result from DVT—is the third leading cause of cardiovascular death in the United States, after myocardial infarction and stroke. The annual incidence of DVT approaches 2 million.1 Silent PE constitutes approximately half of DVT cases, as suggested by studies using ventilation perfusion scanning. The true incidence of PE is not known but is estimated to be 600,000 cases annually,1 with approximately one third of these cases leading to death.2
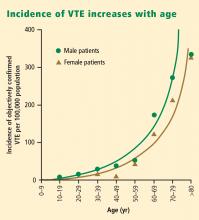
Notably, the incidence of VTE rises at an exponential rate with increasing age after the second decade of life, as shown in Figure 1.2 Given the aging of the US population, this suggests that the clinical and economic impact of VTE will only increase in the years ahead.
DESPITE ESTABLISHED BENEFITS, VTE PROPHYLAXIS REMAINS UNDERUSED
The frequency, clinical impact, and economic impact of VTE make a strong case for VTE prevention. In a 2001 analysis of patient safety practices, the Agency for Healthcare Research and Quality listed appropriate VTE prophylaxis in at-risk patients first in a rating of safety practices with the greatest strength of evidence for impact and effectiveness.4
Despite this recognition of the importance and benefit of VTE prophylaxis, prophylaxis remains highly underutilized. This has been demonstrated in numerous studies; the large epidemiologic investigation by Goldhaber et al using the DVT Free Registry is illustrative.5 This prospective multicenter study enrolled 5,451 consecutive patients with acute DVT documented by venous ultrasonography over a 6month period. Patients were classified as either outpatients or inpatients: outpatients were those who came to the emergency room and were diagnosed with DVT; inpatients were those who developed DVT in the hospital. Of the 2,726 inpatients in the registry, only 42% had received prophylaxis within 30 days prior to their diagnosis of DVT.
Risk extends to the outpatient setting
In a recent population-based analysis, Spencer et al found a similarly low rate of VTE prophylaxis— 42.8%—among 516 patients who had recently been hospitalized and subsequently developed VTE.6 This study also found that VTE was three times as likely in the outpatient setting as in the inpatient setting, and that almost half of the outpatients with VTE had been recently hospitalized. Taken together, these findings indicate that VTE prevention efforts are inadequate both in the hospital and at the time of discharge, when patients’ risk for VTE is still elevated.6,7
VTE PROPHYLAXIS AS AN EMERGING QUALITY MEASURE
Increased recognition of the impact of VTE has prompted accreditation and quality organizations to take interest in VTE risk assessment and prophylaxis as a measure for institutional performance ratings and even reimbursement.
The Joint Commission on Accreditation of Healthcare Organizations and the National Quality Forum have launched a joint project to develop a set of standardized inpatient measures to evaluate hospitals’ practices for the prevention and treatment of VTE.8 The project has pilot-tested several proposed performance measures in dozens of volunteer hospitals, including measures of whether VTE risk assessment is performed and VTE prophylaxis is initiated (if indicated) within 24 hours of admission to the hospital or to the intensive care unit. Hospitals participating in the pilot program are required to report their rates of potentially preventable hospital-acquired VTE.
Similarly, the ongoing Surgical Care Improvement Incidence of VTE increases with age Project (SCIP) has targeted VTE prophylaxis as one of a handful of priority areas for reducing surgical complications. As a national quality partnership of organizations sponsored by the Centers for Medicare and Medicaid Services (CMS), SCIP set a national goal in 2005 to reduce preventable surgical morbidity and mortality by 25% by 2010.9
The stakes of the SCIP initiative are high in both clinical and financial terms. CMS mandated that hospitals report on three SCIP quality measures in 2007 in order to receive full Medicare reimbursement in 2008. Of the three measures, two involved VTE prophylaxis: (1) how often VTE prophylaxis was ordered for surgical patients when indicated, and (2) how often appropriate surgical patients received prophylaxis postoperatively. Moreover, beginning October 1, 2008, CMS will no longer reimburse hospitals for cetain preventable conditions, and DVT and PE are being considered for inclusion in this list of conditions excluded from reimbursement.10
PROPHYLAXIS RATES CAN BE IMPROVED
Fortunately, there is evidence that interventions to increase awareness may increase the rate of VTE prophylaxis. Stinnett et al reported that education, in the form of hospital-specific data on VTE rates and implementation of risk-stratification guidelines, increased the use of VTE prophylaxis in high-risk hospitalized medical patients at a tertiary care center from a preintervention rate of 43% to a postintervention rate of 72%.11
In addition to educational interventions, formalized risk-assessment tools, in the form of electronic alerts, offer another strategy that may increase rates of VTE prophylaxis. The promise of this approach was demonstrated in a study at Brigham and Women’s Hospital in Boston, in which 2,506 hospitalized patients at risk for VTE were randomly assigned to either an intervention group, in which physicians received a computer alert about the patient’s VTE risk, or a control group, in which no alert was issued.12 The rate of VTE prophylaxis was more than twice as high in the intervention group as in the control group (33.5% vs 14.5%; P < .001), and the 90-day incidence of VTE was reduced from 8.2% in the control group to 4.9% in the intervention group (P = .001).