Reconstruction options following breast conservation therapy
ABSTRACT
Women who have had breast conservation therapy for malignancy are candidates for various surgical techniques for immediate or delayed breast reconstruction. These include local tissue rearrangement, therapeutic reduction mammaplasty, and various flap reconstruction procedures. Each technique has advantages and disadvantages, and individual patient factors, particularly breast size and resection defect size, should drive the choice among procedures. Immediate reconstruction (at the time of breast conservation surgery) is preferred over delayed reconstruction, for multiple reasons. Patients tend to be satisfied with the cosmetic outcome of these procedures, but thorough patient counseling and preop-immediate or erative planning is critical to a good result.
Flap reconstruction
Flap reconstruction is indicated in patients who have significant breast volume deficit after resection and have insufficient adjacent tissue for local tissue recruitment and rearrangement. This method of reconstruction is based on an axial blood supply, which means that a specific vascular pedicle is responsible for a given distribution of tissue. For this purpose, flaps can be either myocutaneous (muscle-skin flaps), fasciocutaneous (fascia, subcutaneous tissue, and skin) or adipocutaneous (containing fat and skin). Examples include the latissimus dorsi myocutaneous flap, the transverse thoracoepigastric skin flap, and the lateral thoracic adipocutaneous flap.4–6
The latissimus dorsi myocutaneous flap is used most often, especially when more than 25% of the breast volume has been resected. Since a large volume of tissue is removed, either the tumor and a margin can be resected or a nipple-sparing subcutaneous mastectomy may be performed10 (nipple-sparing mastectomy would not be breast-conserving and has been discussed earlier in this supplement). This myocutaneous flap is based on the thoracodorsal vessels and was first described for volume replacement after breast-conserving surgery by Noguchi et al.13 A benefit of this flap is that most patients do not need reduction of the contralateral breast for symmetry, as the flap usually provides adequate tissue volume.4 This is beneficial for the patient, as she is not exposed to the potential complications of an operation on the contralateral breast.
The lateral thoracic adipocutaneous flap is another option. This flap has the benefit of sparing the muscle while using skin and fat from the axillary region. It can be based on one of three vascular pedicles that have been shown to be reliable as a sole blood supply. The most common pedicle for this technique is the thoracodorsal artery, as the main blood supply for the thoracodorsal artery perforator flap. This flap provides a potentially large amount of tissue for use and affords patients the chance to have a redundant roll of axillary tissue removed. This tissue can be used alone for reconstruction or in conjunction with a breast implant.6
One drawback of the latissimus dorsi flap is the potential for mismatch of skin color and texture when there is a need to address a significant skin deficit on the breast. Replacing a whole aesthetic unit, as opposed to only a small skin paddle, can minimize this potential; thus, using a larger amount of skin may provide a better aesthetic result. Rarely, if there is no skin defect, the muscle alone can be used, with no skin component.5 The lateral thoracic flap, on the other hand, may be more similar in skin color and texture to the native breast and may allow the scar to be better hidden in the axilla than is the case with the latissimus dorsi flap.6 Any type of flap presents potential donor site problems as well as breast complications (discussed below).
Flap reconstruction broadens the application of breast conservation therapy to women who would not otherwise be candidates because of the large volume of tissue they need to have removed.2 Oncoplasty reconstruction also allows the oncologic surgeon to be more aggressive with tissue removal without concerns about compromising the aesthetic outcome. Patients with small to moderate breasts are therefore candidates for flap reconstruction, as even modest resections in such patients result in a large volume of tissue loss and the need for additional tissue to reconstruct the breast.14 Any of the aforementioned flaps are advantageous, as they are in close proximity to the breast and can readily be used for reconstruction.6
CHOICE OF TECHNIQUE
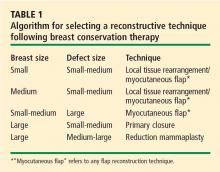
Many factors contribute to the choice among reconstructive methods for a particular patient after breast conservation therapy.
Tumor location plays a significant role. Kronowitz et al described using breast reduction as their primary reconstructive modality, particularly for tumors of the upper inner, upper outer, and lower inner quadrants of the breast.4 They used flap reconstruction only for outer-quadrant tumors, and they found that tumors of the lower outer quadrant were the largest and lent themselves to local tissue rearrangement, often with axillary tissue.4 Centrally located tumors usually require removal of the nipple-areola complex and can be challenging to reconstruct. The techniques include either (1) direct closure with some degree of local tissue remodeling, or (2) reduction mammaplasty. The majority of patients with centrally located tumors will need contralateral breast reduction for symmetry14 and nipple-areola reconstruction at a later date.
The size of the defect created by the tumor resection also significantly affects the choice of technique, as does the patient’s preoperative brassiere size. In the analysis by Kronowitz et al, defects smaller than 20% of the overall breast size were found to be amenable to breast reduction, whereas larger defects were reconstructed with flaps or local tissue rearrangement.4 Also, women with a brassiere cup size of D or larger tended to undergo breast reduction, whereas those with a size smaller than D underwent local tissue rearrangement or flap reconstruction.4
COMPLICATIONS
Complications of breast surgery include seromas (of the breast as well as the donor site when a flap is used), nipple necrosis, wound dehiscence, infection, hematoma, fat necrosis, and mastectomy flap necrosis. Postoperative hematomas and superficial wound infections tend to occur in the immediate postoperative period (usually within the first few days), whereas the other complications mentioned may take 1 to 2 weeks to develop. These complications are common to all breast operations and are not specific to reconstruction after breast conservation therapy.
Postoperative complications vary in frequency but are more common when reconstruction is delayed.4,7 They also vary depending on the reconstructive technique. Donor-site seromas and fat necrosis are most common with immediate reconstruction using a flap; wound dehiscence is most common with delayed local tissue rearrangement; and breast seroma is most common with delayed reduction mammaplasty.4
Other issues to consider include the possible delay in adjuvant therapy in patients who experience wound healing problems, especially in those who are obese, who smoke, or who undergo therapeutic mammaplasty.15,16 Moreover, operative time is increased with oncoplasty as compared with simple wide local excision, which increases patients’ exposure to anesthesia and thereby raises the risk of complications, particularly in older patients with comorbidities.16