Hemorrhoids: A range of treatments
Release date: September 1, 2019
Expiration date: August 31, 2020
Estimated time of completion: 1 hour
Click here to start this CME/MOC activity.
ABSTRACT
Hemorrhoids are a common reason for office visits. Each patient is unique, and with a range of treatments available, treatment can be individualized. This article reviews the diagnosis and decision-making process for individualized treatment.
KEY POINTS
- Hemorrhoids account for more than 3.5 million office visits annually.
- Most patients present with painless rectal bleeding, but this can also be a sign of colorectal cancer, which needs to be ruled out.
- Fiber supplements along with dietary and lifestyle changes are recommended for all patients with hemorrhoids regardless of symptom severity.
- Hemorrhoids are graded on a scale of I (least severe) through IV (most severe). Office-based treatments are effective for grades I, II, and some grade III hemorrhoids. Surgical excision is the standard for high-grade hemorrhoids.
SURGERY
Although nonsurgical treatments have substantially improved, surgery is the most effective and strongly recommended treatment for patients with high-grade internal hemorrhoids (grades III and IV), external and mixed hemorrhoids, and recurrent hemorrhoids.
The most popular surgical options are open or closed hemorrhoidectomy, stapled hemorrhoidopexy, and Doppler-guided hemorrhoidal artery ligation. Each has different success rates and different complication profiles, which need to be discussed with the patient.
Overall, surgery is associated with more adverse effects than office-based treatments or medical management. Postoperative pain is the most common complaint, but anal stricture (rare) or incontinence may occur due to excessive tissue excision and damage to the sphincter muscles. These can be avoided by maintaining the normal anoderm between excisions, by not excising all hemorrhoid sacs at once if the patient has extensive lesions, and by performing a careful dissection in the submucosal plane.
,Patients with profuse bleeding or an underlying bleeding abnormality are best managed with surgical approaches performed in an operating room.
Excisional surgical hemorrhoidectomy
Excision of the hemorrhoidal sac, the most conventional surgical technique, is generally reserved for prolapsing disease. The recurrence rate after excisional hemorrhoidectomy is significantly lower than with any other approach.29
Excisional hemorrhoidectomy can be performed using either an open approach, in which the edges of the mucosal defect are not reapproximated, or a closed approach, in which they are. In a systematic review, Bhatti et al30 compared open vs closed techniques and found that the closed technique resulted in less postoperative pain, better wound healing, and less bleeding. Rates of recurrence, postoperative complications, and surgical site infection and lengths of stay were comparable with either procedure.
Overall, excisional hemorrhoidectomy is associated with higher pain scores than any other surgical method.29 Recently, the use of electrodiathermy energy devices, also described as electrosurgical vessel-sealing devices, have further improved overall patient satisfaction.31
Multiple painful hemorrhoidal sacs require a careful surgical approach, as extensive resection may cause widespread fibrosis and stricture. As with anal stricture, fecal incontinence can be prevented by careful dissection. However, already existing incontinence is not a contraindication for the surgery.
Doppler-guided hemorrhoidal artery ligation
Doppler-guided hemorrhoidal artery ligation involves using a Doppler probe to find and ligate individual hemorrhoidal arteries. Additionally, mucopexy (transanal rectoanal repair) is performed to relocate the prolapsing tissue. Avital et al32 reported that at 1 year after this procedure, recurrence rates were 5.3% for grade II hemorrhoids and 13% for grade III hemorrhoids. At 5 years, recurrence rates were 12% for grade II and 31% for grade III.
To date, this procedure appears to be suitable for grade I, II, and III hemorrhoids, especially for grade II, but more studies are needed to prove its efficacy and recurrence rates for more advanced lesions. Although this technique has a high morbidity rate (18%), primarily pain or tenesmus, it causes less postoperative pain than other surgical methods.33 Overall, it has the potential to become a favored treatment.
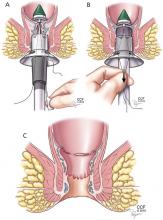
Stapled hemorrhoidopexy
Although pain scores are lower with stapled hemorrhoidopexy than with excisional hemorrhoidectomy, this procedure is not superior in terms of recurrences.34,35 Also, practitioners should be careful about specific complications of stapled hemorrhoidopexy, such as rectovaginal fistula, anal stenosis, or sphincter injuries. These specific complications should be clearly explained to patients, and necessary information should be given to patients upon discharge. The primary care physician should also be careful about fistulas and stenoses in this particular patient population.