Hemorrhoids: A range of treatments
Release date: September 1, 2019
Expiration date: August 31, 2020
Estimated time of completion: 1 hour
Click here to start this CME/MOC activity.
ABSTRACT
Hemorrhoids are a common reason for office visits. Each patient is unique, and with a range of treatments available, treatment can be individualized. This article reviews the diagnosis and decision-making process for individualized treatment.
KEY POINTS
- Hemorrhoids account for more than 3.5 million office visits annually.
- Most patients present with painless rectal bleeding, but this can also be a sign of colorectal cancer, which needs to be ruled out.
- Fiber supplements along with dietary and lifestyle changes are recommended for all patients with hemorrhoids regardless of symptom severity.
- Hemorrhoids are graded on a scale of I (least severe) through IV (most severe). Office-based treatments are effective for grades I, II, and some grade III hemorrhoids. Surgical excision is the standard for high-grade hemorrhoids.
OFFICE-BASED TREATMENTS
Office-based treatments—rubber band ligation, infrared photocoagulation, and sclerotherapy—are commonly used for grade I, II, and III hemorrhoids that have not responded to conservative management. The primary goal of these treatments is to decrease blood flow into the hemorrhoidal sac.
Even though office-based treatments are highly effective and major complications are uncommon, recurrence rates can be high, requiring patients to undergo additional treatments. Moreover, septic complications can occur, so patients should be closely observed for fever and urinary problems. Pain is a common symptom after office-based treatments, and bleeding may also occur.
The ASCRS guidelines strongly recommend office-based treatments for patients with grade I and II hemorrhoids, and for some with grade III hemorrhoids.3
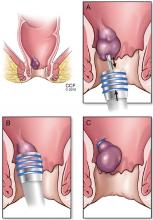
,Rubber band ligation
Iyer et al18 reported that patients on warfarin therapy had up to a 9 times higher risk of postprocedural bleeding, and patients on aspirin had a risk up to 3 times higher. Therefore, whether patients on anticoagulant therapy should undergo this procedure is unclear.
A Cochrane database review19 found this technique effective for hemorrhoid grades I through III, although some patients with grade III hemorrhoids may benefit more from excisional hemorrhoidectomy, which is associated with a lower recurrence rate than rubber band ligation.
Brown et al20 performed a randomized controlled trial comparing hemorrhoidal artery ligation and rubber band ligation for symptomatic hemorrhoids in 372 patients with grade II and III hemorrhoids. Postprocedural pain scores on days 1 and 7 were significantly lower with rubber band ligation, but recurrences were more common (49% vs 30%, P = .0005, respectively).
Overall, rubber band ligation is an excellent option for grade II hemorrhoids, as it is easy to perform, is associated with low pain scores, and can be used to treat recurrences.
Infrared photocoagulation
In this procedure, an infrared probe produces heat to induce coagulation, fibrosis, and ultimately necrosis of the protruding tissue in the hemorrhoidal cushions.21 Even though its use was initially directed at grade I and II hemorrhoids, recent reports showed acceptable results for grades III and IV.22,23 A randomized controlled trial comparing infrared photocoagulation and rubber band ligation in 94 patients found that both procedures were well accepted and highly effective; however, patients had better pain scores with photocoagulation in the first 24 hours after the procedure (P < .05).24
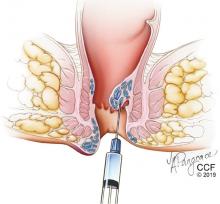
Sclerotherapy
The injection can cause prostatic abscess and sepsis, although this is rare.25 Nevertheless, high fever and postprocedural pain should be carefully evaluated.
There have been few randomized trials of sclerotherapy, but success rates so far have been higher for grade I hemorrhoids than for grades II and III.26–28 It is the preferred method for patients who have bleeding abnormalities caused by medications or other diseases (eg, cirrhosis).