Perioperative management of anemia: Limits of blood transfusion and alternatives to it
ABSTRACT
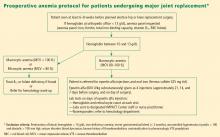
Perioperative anemia is associated with excess morbidity and mortality. Transfusion of allogeneic blood has been a long-standing strategy for managing perioperative anemia, but the blood supply is insufficient to meet transfusion needs, and complications such as infection, renal injury, and acute lung injury are fairly common. Further, data suggest that mortality and length of stay are worsened with liberal use of transfusion. Medical alternatives to transfusion include iron supplementation and erythropoiesis-stimulating agents (ESAs). Though ESAs reduce the need for perioperative blood transfusion compared with placebo, they are associated with an increased risk of thrombotic events in surgical patients. Cleveland Clinic has been developing a blood management program aimed at reducing allogeneic blood exposure for greater patient safety; the program has achieved some reduction in blood utilization in its first 7 months.
KEY POINTS
- Anemia is a potent multiplier of morbidity and mortality risk, including in the perioperative setting.
- The Joint Commission plans to implement a performance measure on blood management in the near future.
- While the safety of the blood supply has improved markedly from the standpoint of infection transmission, other risks from transfusion persist, including transfusion-related acute lung injury and emerging infections.
- The preoperative evaluation should elicit a history of bleeding tendencies, previous transfusions, and symptoms of anemia. Medications should be reviewed with an eye toward those that may need to be stopped to avoid a predisposition to bleeding (eg, antiplatelets, anticoagulants).
- Use of ESAs minimizes the need for blood transfusion in patients undergoing orthopedic and other surgeries, but they raise the risk of thromboembolism in the absence of prophylactic anticoagulation.
TECHNOLOGICAL OPTIONS AND OTHER STRATEGIES
Autologous blood donation: A practice in decline
In cases of elective surgery, autologous blood donation can be used to protect against disease transmission and overcome the challenge of blood type compatibility. Preoperative autologous donation of blood has been a prevalent practice, but its use is declining. One reason is that waste is high (approximately 50% at Cleveland Clinic), which makes this practice more costly than is often realized. Also, autologous blood donation increases the likelihood that the patient will be anemic on the day of surgery, so that he or she may still need allogeneic blood after all, defeating the initial purpose. Despite these limitations, preoperative autologous blood donation remains a useful option for a subset of patients with multiple antibodies for whom donor blood may be difficult to obtain.
Cell salvage
Cell salvage is an innovative technology that recovers the patient’s own blood (after being shed from the surgical incision) for transfusion after filtering and washing. It is particularly well suited to procedures that involve massive blood loss. Cell savage requires technical expertise, however, and involves costs associated with both the machine and disposables.
Restricted postoperative phlebotomy
Phlebotomy accounts for a significant amount of blood loss, especially in intensive care patients with arterial lines. The equivalent of 30% of total blood transfused has been reported to be lost to phlebotomy during an intensive care unit stay.36 Triggers for transfusion cannot be assigned universally based on blood loss from phlebotomy but must consider the patient’s hemodynamic status, cardiac reserve, and other clinical characteristics.
PROMOTING RESPONSIBLE BLOOD PRODUCT USE
Blood is expensive, and in recent years hospitals have experienced increases in the cost of blood and blood products. To promote responsible blood use, we have developed a multipronged approach to blood management at Cleveland Clinic. The program’s cornerstone is increased awareness of the risks associated with blood transfusions. The emphasis is on educating staff physicians and other caregivers about the appropriate use of blood products. We also have implemented a new policy requiring staff authorization for all blood requested in nonemergency situations. Additionally, requests for blood components require adherence to an indication-based ordering process. Finally, data about blood use are shared transparently among physicians, encouraging good clinical practice.
In the first 7 months of the program, we observed decreased utilization of blood products in the inpatient setting. Notably, the reduction in blood use was significantly greater in the surgical population than in the medical population.
CONCULSIONS
Anemia is associated with increased morbidity and mortality in the perioperative setting. Perioperative blood transfusion is one method of raising hemoglobin levels in anemic surgical patients, but it increases perioperative morbidity in the form of acute transfusion reactions, immunosuppression, postoperative infection, and longer hospital stays. Moreover, blood collection continues to lag blood demand. For these reasons, most relevant major medical organizations—including the Association of Blood Banks, the American Red Cross, and the FDA—advise that red blood cell–containing components should not be used to treat anemias that can be corrected with medications. These medical alternatives—all of which can be used in the perioperative setting—include iron supplementation, vitamin B12, and ESAs in select patient groups.
DISCUSSION
Question from the audience: Are there risks involved with autologous blood donation? Are different hemoglobin thresholds used when a patient’s own blood is used?
Dr. Kumar: As I mentioned, preoperative autologous donation is a technique that is less frequently used in our hospital. Autologous transfusion is considered safe only for patients who come to the clinic with normal hemoglobin values. Some patients may not have recovered from their blood loss by the time they come to surgery, so you end up needing to give them more blood because they started out anemic.
Question from the audience: Is there risk to giving patients back their own blood? Do you have to worry about transfusion-induced lung injury, sepsis, or other complications?
Dr. Kumar: As with allogeneic blood, the risk of clerical or clinical error exists with autologous blood: it too needs to be kept on the shelf, taken out, and infused, and the risk of sepsis remains the same.