Perioperative management of warfarin and antiplatelet therapy
ABSTRACT
Perioperative management of patients on warfarin or antiplatelet therapy involves assessing and balancing individual risks for thromboembolism and bleeding. Discontinuing anticoagulant and antiplatelet therapy is usually necessary for major surgery but increases the risk of thrombotic events. Bridge therapy, the temporary perioperative substitution of low-molecular-weight heparin or unfractionated heparin in place of warfarin, is an effective means of reducing the risk of thromboembolism but may increase the risk of bleeding. The timing of warfarin withdrawal and timing of the preoperative and postoperative components of bridge therapy are critical to balancing these risks. Perioperative management of antiplatelet therapy requires special care in patients with coronary stents; the timing of surgery relative to stent placement dictates management in these patients.
KEY POINTS
- Determining when and how to use bridge anticoagulation therapy depends on the patient’s risk for thromboembolism, which is in turn based on the indication for warfarin—ie, a mechanical heart valve, atrial fibrillation, or prior venous thromboembolism.
- Factor patient preference into whether and how to use bridge therapy: many patients are more concerned about stroke risk than bleeding risk, regardless of the relative frequency of these events.
- Anticoagulation with warfarin often does not need to be interrupted for patients undergoing minor surgery, such as some ophthalmic, dental, dermatologic, and gastrointestinal procedures.
- Premature discontinuation of antiplatelet therapy in surgical patients with recent coronary stent placement significantly raises the risk of catastrophic perioperative stent thrombosis.
PERIOPERATIVE MANAGEMENT OF ANTIPLATELET THERAPY: TYPE OF AGENT MATTERS
Unlike the considerations with warfarin, the timing of preoperative discontinuation of antiplatelet therapy in patients undergoing noncardiac surgery depends on the type of agent used and its pharmacokinetic actions. Commonly used antiplatelet drugs include aspirin, the thienopyridine agent clopidogrel, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Aspirin works by irreversibly inhibiting platelet cyclooxygenase. The circulating platelet pool is replaced every 7 to 10 days, so aspirin therapy should be discontinued 7 to 10 days before surgery.1
NSAIDs reversibly inhibit platelet cyclooxygenase. Knowing whether a patient is using short- or long-acting NSAIDs is important for determining when to discontinue therapy. For a short-acting NSAID such as ibuprofen, discontinuation 24 hours before surgery may be adequate to normalize platelet function.1,30
Thienopyridines inhibit adenosine diphosphate receptor–mediated platelet activation and aggregation. Short-acting thienopyridines may be discontinued 24 hours before surgery, but long-acting agents such as clopidogrel should be stopped 7 days prior to surgery (including when used with aspirin as dual antiplatelet therapy),1 although some outcomes data suggest that 5 days may be sufficient.31
All of these agents should be resumed as soon as adequate hemostasis is achieved after surgery. The ACCP guidelines on perioperative management of antithrombotic therapy recommend resumption of aspirin at the usual maintenance dose the day after surgery, but they make no specific recommendations on when to resume other antiplatelet drugs.1
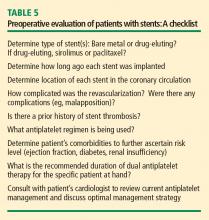
ANTIPLATELET THERAPY: SPECIAL CONSIDERATIONS IN PATIENTS WITH STENTS
Patients who are on antiplatelet therapy because they have a coronary stent merit special consideration due to the high risk of thrombosis if therapy is interrupted. The risk of stent thrombosis is especially elevated in the postoperative period, particularly if surgery follows soon after stent placement.
- Relative risks and benefits of stopping versus continuing antiplatelet therapy
- Identification of patients at high risk for a perioperative event after cessation of antiplatelet therapy
- Identification of patients at high risk of bleeding.
Bleeding vs stent thrombosis: Consider relative consequences
The risk of bleeding varies by individual patient. No laboratory tests are available to determine individual bleeding risk, but the risk of perioperative bleeding increases when two or more antiplatelet agents are used, as in dual antiplatelet therapy with aspirin and clopidogrel.31
When balancing risks of bleeding versus thrombotic events, the relative consequences of each event again must be considered. Bleeding is rarely life-threatening in comparison with the potential consequences of stent thrombosis. In a prospective observational study of 2,229 patients who received drug-eluting stents, 29 (1.3%) developed stent thrombosis during 9-month follow-up.32 Among these patients, 20 (69%) had a nonfatal myocardial infarction and 13 (45%) died. The most significant independent risk factor for stent thrombosis was premature discontinuation of antiplatelet therapy (hazard ratio = 89.78 [95% CI, 29.90–260.60]; P < .001). Other independent risk factors included renal failure, bifurcation lesions, diabetes, and low ejection fraction.
Premature interruption of antiplatelet therapy: Why it matters
Abrupt discontinuation of antiplatelet therapy can lead to a rebound effect marked by an inflammatory prothrombotic state, increased platelet adhesion and aggregation, and excessive thromboxane A2 activity. Surgery further increases the prothrombotic and inflammatory state, which, combined with incompletely endothelialized drug-eluting stents, can lead to stent thrombosis and, consequently, myocardial infarction and/or death.33
Timing of surgery after stenting: Getting it right
The US Food and Drug Administration recommends that dual antiplatelet therapy be continued for at least 3 months after placement of a sirolimus-eluting stent and at least 6 months after placement of a paclitaxel-eluting stent. Recent data suggest, however, that this duration of antiplatelet therapy may not be sufficient and that at least 1 year of therapy may be needed.34
A recent joint science advisory from the American College of Cardiology (ACC) and the American Heart Association (AHA) emphasizes the importance of educating providers about the “potentially catastrophic” risks of premature stopping of thienopyridine therapy in patients with coronary stents.34 In addition to recommendations in this joint advisory, the ACC and AHA issued updated guidelines in 2007 on perioperative cardiovascular evaluation and care for noncardiac surgery.35 Below is a summary of recommendations on the timing of surgery following stenting in light of these and other sources:
- Following placement of a bare metal stent, elective and nonurgent procedures should be delayed for at least 1 month, according to the ACC/AHA joint advisory,34 or at least 6 weeks, according to the ACC/AHA guidelines.35 Newer data suggest that the optimal interval for delay is likely to be 3 months.36,37
- For patients with recent (< 6 weeks) bare metal stent placement who require urgent surgery, dual antiplatelet therapy should be continued during the perioperative period.1
- Following placement of a drug-eluting stent, elective and nonurgent procedures should be delayed for at least 12 months.34,35
- For patients with recent drug-eluting stent placement in whom surgery cannot be delayed, dual antiplatelet therapy should be continued without interruption if the stent was placed within the prior 6 months.1,35 If the stent was placed more than 6 months before urgent surgery, aspirin should be continued without interruption (at ≥ 81 mg/day) and clopidogrel should be continued until 5 days before surgery and resumed as soon as possible after surgery (at a loading dose of 300 mg followed by 75 mg/day). If the surgeon is comfortable continuing dual antiplatelet therapy in a patient whose stent was placed 6 to 12 months earlier, that course should be considered.1
It is important to note that the ACC/AHA joint advisory34 and other documents have medicolegal implications, so delaying nonurgent surgery for the periods recommended is the most prudent approach.