Novel antiplatelet strategies in acute coronary syndromes
ABSTRACT
Antiplatelet therapies for the treatment of acute coronary syndromes (ACS) act to interrupt various pathways of platelet activation. Clopidogrel, an established thienopyridine antiplatelet medication, inhibits adenosine diphosphate (ADP)–induced platelet aggregation to a modest degree and with wide variability in platelet response. Accumulating data suggest that a 600-mg loading dose of clopidogrel may help overcome the suboptimal response to the standard 300-mg dose seen in some patients. Prasugrel is a third-generation investigational thienopyridine that demonstrates more potent inhibition of platelet aggregation and more consistent platelet response compared with standard- and high-dose clopidogrel. A large clinical trial showed prasugrel to be superior to standard-dose clopidogrel in reducing ischemic events in patients with ACS scheduled for percutaneous coronary intervention, although prasugrel was associated with a significantly higher risk of major bleeding events. Other investigational antiplatelet agents also display more potent and consistent inhibition of platelet aggregation than is seen with clopidogrel. These include AZD6140, a reversible ADP receptor blocker; cangrelor, a rapidly acting intravenous ADP receptor blocker; and the thrombin receptor antagonist SCH 530348.
KEY POINTS
- There is substantial interpatient variability in the response to clopidogrel.
- In the large TRITON-TIMI 38 trial, the composite rate of death, myocardial infarction, or stroke was reduced by 19% and the rate of stent thrombosis was halved in patients receiving prasugrel compared with standard-dose clopidogrel.
- The risk of major bleeding with prasugrel is highest in patients aged 75 or older, those weighing less than 60 kg, and those with a history of stroke or transient ischemic attack.
- Thrombin receptor antagonists are being studied to see if their use can reduce ischemic events without increasing bleeding.
THROMBIN INHIBITORS
Thrombin plays an important role in platelet activation, and thrombin receptor antagonists may represent a safer means of inhibiting platelet activation relative to traditional antiplatelet agents. This theoretical safety advantage stems from the notion that blocking the action of platelets at the thrombin receptor would preserve platelets’ function as mediators of primary hemostasis. Because thrombin’s activation of platelets should occur only during clot formation, blocking platelet activation at the thrombin receptor would interrupt thrombin’s ability to propagate platelet activation during formation of coronary artery clots.
One agent in this class that is being studied extensively is SCH 530348, an oral thrombin receptor antagonist with potent antiplatelet activity. Its peak antiplatelet potency is achieved within hours when a loading dose is given, and within days without a loading dose. Wearing-off of the action of SCH 530348 takes weeks.24
Inhibition of platelet aggregation with thrombin receptor antagonists is measured in response to the thrombin receptor antagonist peptide (TRAP), not ADP. The proportion of subjects treated with SCH 530348 who achieve greater than 80% inhibition of platelet aggregation to 15 μM of TRAP ranges from 91% (with 0.5 mg of SCH 530348) to 100% (with 1.0 mg and 2.5 mg) at both 30 days and 60 days.25
,Clinical effects in placebo-controlled trials
SCH 530348 was studied in the Thrombin Receptor Antagonist (TRA)–PCI trial, a dose-ranging study in which patients were randomized to one of three oral loading doses of the study drug (10 mg, 20 mg, or 40 mg) on top of a clopidogrel loading dose before undergoing cardiac catheterization for planned PCI; patients were then randomized to one of three maintenance doses of SCH 530348 (0.5 mg, 1.0 mg, or 2.5 mg) or placebo (depending on loading therapy) for 60 days.25
Among the 573 patients undergoing PCI , the rate of TIMI major or minor bleeding was not significantly higher with any dose of SCH 530348 compared with placebo,25 supporting the hypothesis that thrombin receptor antagonism inhibits platelet aggregation without a significant increase in bleeding.
Although the TRA-PCI study was not powered to detect differences in clinical event rates, a reduction in the rate of major adverse cardiovascular events was observed in a dose-dependent manner with SCH 530348 compared with placebo in the PCI cohort.25
On the basis of the TRA-PCI trial, a pair of phase 3 trials of SCH 530348 have been launched—the Thrombin Receptor Antagonist in Secondary Prevention of Atherothrombotic Ischemic Events (TRA 2°P-TIMI 50) study and the Thrombin Receptor Antagonist for Clinical Event Reduction in ACS (TRA-CER) study.
TRA 2°P-TIMI 50 is a multinational double-blind study enrolling 19,500 patients with prior MI or stroke or with existing peripheral arterial disease. Patients are being randomized to placebo plus standard medical care (including aspirin and clopidogrel) or to 2.5 mg of SCH 530348 once daily plus standard medical care. The primary end point is the composite of cardiovascular death, MI, urgent coronary revascularization, or stroke.26
TRA-CER is a multinational double-blind study with planned enrollment of 10,000 patients with non-ST-segment-elevation MI. Patients are being randomized to placebo plus standard medical care (including aspirin or clopidogrel) or to SCH 530348 (using the oral 40-mg loading dose and a maintenance dose of 2.5 mg once daily) plus standard medical care. The primary end point is the composite of cardiovascular death, MI, rehospitalization for ACS, urgent coronary revascularization, or stroke. The key secondary end point is the composite of cardiovascular death, MI, or stroke.27
COMPARATIVE CONSIDERATIONS
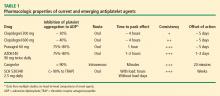
Inhibition of platelet aggregation
Clopidogrel achieves about 30% inhibition of platelet aggregation to ADP at its current FDA-approved loading dose of 300 mg and about 40% inhibition when its dose is doubled to 600 mg. These levels of inhibition are increased to 75% to 80% by clopidogrel’s fellow thienopyridine prasugrel, and this increase is attributable to prasugrel’s more efficient metabolism from prodrug to active metabolite. The reversible P2Y12 receptor antagonist AZD6140 achieves a comparable 75% to 80% inhibition of platelet aggregation. The parenterally administered P2Y12 receptor antagonist cangrelor achieves greater than 90% inhibition, as does the oral thrombin receptor antagonist SCH 530348, although the latter agent’s inhibition is to the agonist TRAP rather than ADP.
Time to peak effect
The time to peak effect with clopidogrel is approximately 4 hours regardless of the loading dose used (300 mg or 600 mg); this is substantially reduced with all of the investigational agents except SCH 530348. The novel agents’ reduced time to peak effect can offer advantages in speeding patients’ readiness to undergo catheterization procedures. This is particularly true for the IV agent cangrelor, which achieves its peak effect within minutes, although the 1-hour to 2-hour time frame with oral agents prasugrel and AZD6140 also would usually obviate any need to delay catheterization.
Consistency of platelet response
Standard-dose clopidogrel has the least consistency of platelet response among the therapies reviewed. Although increasing the clopidogrel dose yields somewhat greater consistency in response, it is still lower than the very high degrees of consistency observed with all of the novel compounds, each of which appears to achieve the same degree of inhibition of aggregation in virtually all patients.
Offset of effect
Both of the thienopyridines—clopidogrel and prasugrel—have an offset of effect of about 5 days, which requires delay of surgery, if possible, for several days in patients taking these agents. This is not an issue for the reversible oral agent AZD6140, whose offset of action takes just 1 to 2 days. While this rapid wearing-off of effect translates to a potential advantage for AZD6140, it also poses the potential drawback that a missed dose or two may leave the patient exposed to the risk of a thrombotic event. Cangrelor’s rapid offset of 20 minutes promotes its envisioned use as a catheterization lab–based medication like the glycoprotein IIb/IIIa inhibitors that can be started right before a PCI procedure and stopped immediately afterward. Because SCH 530348 has a very long half-life and thus a weeks-long washout period, the practicality of its use may depend on the hypothesis that thrombin receptor antagonists do not interfere with primary hemostasis, which is supported by data to date but remains to be definitively confirmed.
CONCLUSIONS
Clopidogrel achieves modest platelet inhibition with wide variability in response. Higher doses of clopidogrel achieve modestly greater degrees of inhibition than standard doses, and appear to result in a decreased rate of ischemic events. Although higher doses of clopidogrel have been embraced by some clinicians, we await definitive phase 3 trial evidence of net benefit before making high-dose clopidogrel the new standard of care.
Compared with clopidogrel, the investigational thienopyridine prasugrel is a more potent and consistent blocker of the ADP receptor. It results in a decreased rate of ischemic events relative to clopidogrel, including a 50% reduction in the rate of stent thrombosis, but is associated with an increased rate of bleeding. If prasugrel is approved for marketing, its use should be avoided in patients with a history of stroke or TIA, and avoidance or dose adjustment may be necessary in patients aged 75 years or older and in patients weighing less than 60 kg.
Other novel antiplatelet agents being evaluated for use in patients with ACS—the reversible oral ADP receptor blocker AZD6140, the rapid-acting IV ADP receptor blocker cangrelor, and oral thrombin receptor antagonists—offer potential advantages that need to be examined in the context of large-scale clinical trials.