Treatment Options for Stable Chronic Obstructive Pulmonary Disease: Current Recommendations and Unmet Needs
Introduction
Chronic obstructive pulmonary disease (COPD) is common, often seen in primary care daily practice, and places a substantial burden on patients, their families, and society.1-4 Although dyspnea, cough, wheezing, chest tightness, and/or sputum production are typical symptoms of COPD, some patients present with less obvious issues, such as a highly sedentary lifestyle, adjusted to match their limitations and fatigue.5-7
Both pharmacologic and nonpharmacologic treatment options can reduce symptoms, treat comorbidities, prevent exacerbation, and improve quality of life, exercise tolerance, and health status in patients with COPD.3 Patients require initial therapy based on symptoms, history, and their own treatment goals, with regular monitoring to determine when to enhance or discontinue unnecessary therapy, and when to refer to a pulmonologist.
Primary care physicians manage the care of approximately 80% of patients with COPD.8 This provides the opportunity to engage patients in management goal-setting that facilitates more tailored treatments, and can improve adherence to therapy, which is historically poor in patients with COPD, thereby improving outcomes.9-11
Current COPD management guidelines
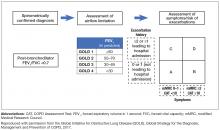
Both the Global Initiative for Obstructive Lung Disease (GOLD) and COPD Foundation guidelines recommend individualized care for patients with COPD.3,12 This individualized care is based on comprehensive assessment of symptoms (including assessment of whether symptoms are persistent or worsening) and/or continuation of exacerbations to escalate therapy. COPD phenotypes, such as individuals with frequent exacerbations, chronic bronchitis, and asthma–COPD overlap syndrome (ACO) can also guide treatment.13-15
GOLD 2017 strategy: key updates
- GOLD A – low symptoms, low exacerbation frequency
- GOLD B – high symptoms, low exacerbation frequency
- GOLD C – low symptoms, high exacerbation frequency
- GOLD D – high symptoms, high exacerbation frequency.
Postbronchodilator spirometry confirms the diagnosis of COPD by a forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ratio of less than 0.7, and denotes levels of airflow limitation severity based on the postbronchodilator FEV1 percentage predicted (Figure 1). Repeated spirometry assessment can identify individuals with rapidly declining lung function who are appropriate for referral to a pulmonologist.
Nonpharmacologic treatment approaches
Smoking cessation and pulmonary rehabilitation are central to effective COPD disease management.3 Smoking cessation has the greatest capacity to influence the natural history of COPD.3 Nicotine replacement products, as well as varenicline and bupropion, have been shown to increase long-term smoking cessation rates.16
Pulmonary rehabilitation (which includes exercise training, education, and self-management interventions aimed at behavior change) should be considered a fundamental part of COPD care.3 Pulmonary rehabilitation is recommended for any COPD patient of GOLD grades B–D (postbronchodilator FEV1/FVC ratio <0.70 and FEV1 <80% of predicted).3 The 2015 Cochrane Review of pulmonary rehabilitation for COPD assessed 65 randomized controlled trials involving 3822 participants, and concluded that pulmonary rehabilitation relieved dyspnea and fatigue, resulting in statistically improved functional exercise, maximal exercise capacity, and quality of life.17 Inclusion of pulmonary rehabilitation in treatment regimens may provide greater benefit than other more commonly used therapies alone.17
Long-term oxygen therapy has been shown to improve survival in COPD patients with severe resting hypoxemia (defined as a partial pressure of arterial oxygen [PaO2] of ≤55 mm Hg, or an oxyhemoglobin saturation level [SpO2] of ≤88%18), and is recommended in the current GOLD guidelines for selected patients.3 However, there is no clinical evidence demonstrating a mortality benefit with oxygen therapy in patients with stable COPD who have only moderate arterial oxygen desaturation (PaO2 of 56–59 mm Hg or SpO2 between 88%–90%18) at rest or with exercise.3 The Long-Term Oxygen Treatment Trial (LOTT) investigated the impact of the prescription of long-term supplemental oxygen in 738 patients with COPD and moderate resting (SpO2 between 89%–93%) or exercise-induced (SpO2 ≥80% for ≥5 min and <90% for ≥10 seconds during exercise) desaturation. Long-term oxygen supplementation did not result in either a longer time to death or first hospitalization.19 In a Cochrane Review published in 2016, Ekström et al conclude with moderate confidence that oxygen can relieve breathlessness when given during exercise to mildly hypoxemic and nonhypoxemic individuals with COPD, but does not improve health-related quality of life.20 Consultation with a pulmonologist is appropriate if when and how to prescribe oxygen therapy is not clear.