Update on the management of venous thromboembolism
ABSTRACT
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism, is a common cardiovascular disease associated with significant morbidity ranging from painful leg swelling, chest pain, shortness of breath, and even death. Long-term complications include recurrent VTE, postpulmonary embolism syndrome, chronic thromboembolic pulmonary hypertension, and postthrombotic syndrome (PTS). Management of VTE requires immediate anticoagulation therapy based on a risk assessment for bleeding. Direct oral anticoagulants (DOACs) have become an important option for patients as reflected in the most recent American College of Chest Physician treatment guidelines.
KEY POINTS
- VTE treatment should begin immediately with heparin, low-molecular-weight heparin (LMWH), fondaparinux, or the DOACs (rivaroxaban or apixaban) in patients deemed appropriate based on a risk assessment for bleeding.
- For patients with VTE and no cancer, long-term treatment with dabigatran, rivaroxaban, apixaban, or edoxaban is recommended over the vitamin K antagonists (VKA).
- LMWH is recommended for the long-term treatment of VTE in patients with cancer.
- For extended-duration anticoagulation, the DOACs (dabigatran, rivaroxaban and apixaban) and the VKA antagonists are options.
- Compression stockings are no longer recommended for prevention of PTS in patients with acute DVT but may be beneficial symptomatically.
Surgical interventions: Pulmonary embolectomy and IVC filters
Pulmonary embolectomy. According to ACCP guidelines, surgical pulmonary embolectomy for the initial treatment of PE is reserved for patients with massive PE (documented angiographically, if possible), shock despite heparin and resuscitation efforts, and failure of thrombolytic therapy or a contraindication to its use.4 To date, there have been no randomized trials evaluating this procedure. Pooled data published by Stein et al29 reported a 20% operative mortality rate in patients undergoing pulmonary embolectomy between 1985 and 2005 compared with 32% in patients undergoing the procedure before 1985. A more recent retrospective review of 214 patients undergoing surgical embolectomy for massive and submassive PE reported an in-hospital mortality rate of 11.7%, with the highest death rate (32.1%) in patients who had a preoperative cardiac arrest.30 The use of surgical embolectomy has also been reported in patients with intermediate-risk to high-risk conditions (defined as elevated biomarkers and evidence of right heart strain on computed tomographic angiography or echocardiography).19
IVC filters. Current guidelines recommend against routine use of IVC filters for patients with DVT or PE who are able to be treated with anticoagulants.3 Absolute indications for the placement of IVC filters include a contraindication to anticoagulation, complications of anticoagulation, and recurrent thromboembolism despite adequate anticoagulant therapy.4 Relative indications for IVC filters are massive PE, iliocaval DVT, free-floating proximal DVT, cardiac or pulmonary insufficiency, high risk of complications from anticoagulation (frequent falls, ataxia), and poor compliance.
Retrievable filters may be considered for situations in which anticoagulation is temporarily contraindicated or there is a short duration of PE risk.31 The current consensus guidelines advise that indications for placing a retrievable IVC filter are the same as for placing a permanent device.31 An IVC filter alone is not effective therapy for VTE, and resumption of anticoagulation is recommended as soon as possible after placement.
DURATION OF TREATMENT
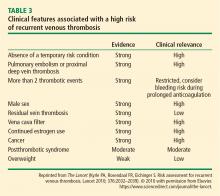
Current guidelines recommend 3 months of anticoagulation (long-term) for patients with an episode of acute proximal or isolated distal DVT of the leg or PE resulting from surgery or a nonsurgical transient cause.3 Patients who have the antiphospholipid syndrome, who are homozygous for factor V Leiden, or who are doubly heterozygous for factor V Leiden and prothrombin gene mutation should be considered for longer (extended) anticoagulation. Extended anticoagulation is also recommended in patients with active cancer and in patients who have unexplained recurrent VTE (Table 2).3
The duration of treatment for unprovoked VTE remains controversial. In the most recent ACCP guidelines, indefinite or extended anticoagulation is indicated for patients with a low or moderate risk of bleeding for a first (and second) unprovoked VTE.4 Patients with a high risk of bleeding with a first (or second) unprovoked VTE that is a proximal DVT of the leg or PE be treated for 3 months.3,4 Three DOACs (rivaroxaban, apixaban, and dabigatran) have extended-duration indications. The 2016 ACCP guidelines suggest aspirin over no treatment for the patient who has decided to stop anticoagulation therapy, although the guidelines do not consider aspirin a reasonable alternative to anticoagulation.34,35 Use of markers such as residual venous obstruction and D-dimer level in conjunction with the DASH score have been studied in an effort to predict the risk of recurrence and thus the duration of anticoagulation.36,37 Residual venous obstruction appears to be less useful than the D-dimer level as an indicator for recurrence. The D-dimer used in conjunction with the DASH prediction score may help to calculate recurrence risk based on the following predictors: abnormal D-dimer 3 weeks after stopping anticoagulation, age under 50, male sex, and hormone use at the time of the VTE.38 DASH score assessment may help physicians decide whether to continue anticoagulation therapy but it has not been shown to be helpful in men.4 A more recent study confirmed the validity of the DASH score with better prediction in patients under age 65. The recurrence rate was higher in the older population, suggesting that this population should be considered for prolonged treatment if the bleeding risk is acceptable.39 Other prediction tools include the Vienna prediction model and the clinical decision rule “Men continue and HER DOO2”—ie, HER = hyperpigmentation, edema, redness; DOO = D-dimer ≥ 250 μg/L, obesity body mass index ≥ 30 kg/m2, old age (≥ 65); 2 = high risk if more than 2 of these factors.40,41
SCREENING AND PREVENTION
Nearly 60% of all VTE events occur in hospitals and nursing homes.42 Yet anticoagulant prophylaxis is used in only 16% to 33% of at-risk hospitalized medical patients compared with 90% of at-risk hospitalized surgical patients.43 Adequate prophylaxis can reduce the incidence of VTE as demonstrated in a meta-analysis involving 19,958 patients, which revealed a 64% reduction in relative risk (RR) of a fatal PE, 58% reduction in RR of a symptomic PE, and a 53% reduction in RR of a symptomatic DVT.43
The consequences of VTE include symptomatic DVT and PE, fatal PE, the cost of investigating symptomatic patients, the risk and cost of treatment (bleeding), PTS, and chronic thromboembolic pulmonary hypertension. Heparin, enoxaparin, and fondaparinux are approved agents for prophylactic but each agent has specific indications. Factor Xa inhibitors, rivaroxaban, and apixaban are approved for use in patients undergoing total knee or hip replacement. More recently, the factor Xa inhibitor, betrixaban, has been approved for VTE prophylaxis for up to 42 days in adult patients hospitalized for acute medical illness.44 For patients with increased bleeding risk who are unable to receive pharmacologic prophylaxis, intermittent pneumatic compression devices or graduated compression stockings should be used.
Compression stockings
Current ACCP guidelines advise against routine use of compression stockings to prevent PTS in patients who have had a DVT.3 While current evidence suggests compression stockings do not prevent PTS, they reduce symptoms of acute or chronic DVT for some patients.