Sexual dysfunction in women: Can we talk about it?
ABSTRACT
Sexual dysfunction in women is common and often goes unreported and untreated. Its management is part of patient-centered primary care. Primary care providers are uniquely positioned to identify and assess sexual health concerns of their patients, provide reassurance regarding normal sexual function, and treat sexual dysfunction or refer as appropriate.
KEY POINTS
- Sexual dysfunction in women is complex and often multifactorial and has a significant impact on quality of life.
- Primary care providers can assess the problem, provide education on sexual health and normal sexual functioning, and manage biological factors affecting sexual function, including genitourinary syndrome of menopause in postmenopausal women and antidepressant-induced sexual dysfunction.
- Treatment may require a multidisciplinary team, including a psychologist or sex therapist to manage the psychological, sociocultural, and relational factors affecting a woman’s sexual health, and a physical therapist to manage pelvic floor disorders.
Many women experience some form of sexual dysfunction, be it lack of desire, lack of arousal, failure to achieve orgasm, or pain during sexual activity.
Sexual health may be difficult to discuss, for both the patient and the provider. Here, we describe how primary care physicians can approach this topic, assess potential problems, and begin treatment.
A COMMON PROBLEM
The age-adjusted prevalence of sexual dysfunction in US women was reported at 44% in the Prevalence of Female Sexual Problems Associated With Distress and Determinants of Treatment Seeking (PRESIDE) study,1 but the prevalence of distress associated with sexual dysfunction was 12%. The most common type of sexual dysfunction reported by women was low sexual desire, a finding consistent with that of another large population-based study.2
While the prevalence of any type of sexual dysfunction was highest in women over age 65,1 the prevalence of distress was lowest in this age group and highest in midlife between the ages of 45 and 65. The diagnostic criteria require both a problem and distress over the problem.
Sexual dysfunction negatively affects quality of life and emotional health, regardless of age.3
LIFESTYLE AND SEXUAL FUNCTION
Various lifestyle factors have been linked to either more or less sexual activity. For example, a Mediterranean diet was associated with increased sexual activity, as were social activity, social support, psychological well-being, self-reported good quality of life, moderate alcohol intake, absence of tobacco use, a normal body mass index, and exercise.4–6 A higher sense of purpose in life has been associated with greater sexual enjoyment.7
Conversely, sexual inactivity has been associated with alcohol misuse, an elevated body mass index, and somatization.4–6
SEXUAL RESPONSE: LINEAR OR CIRCULAR?
Masters and Johnson8 initially proposed a linear model of human sexual response, which Kaplan later modified to include desire and applied to both men and women.9,10 This model presumed that sexual response begins with spontaneous sexual desire, followed by arousal, and then (sometimes) orgasm and resolution.
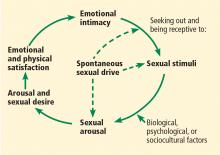
In 2000, Basson11 proposed a circular, intimacy-based model of sexual response in women that acknowledged the complexities involved in a woman’s motivation to be sexual (Figure 1). While a woman may enter the cycle with spontaneous sexual desire, she may also enter it as sexually neutral, with arousal in response to a sexual stimulus. Emotional intimacy is an important part of the cycle, and emotional closeness and bonding with the partner may provide motivation for a woman to enter into the cycle again in the future.
In a Danish survey,12 more people of both sexes said the 2 linear models described their experiences better than the circular model, but more women than men endorsed the circular model, and more men than women endorsed a linear model.
In evaluating women who complain of low sexual desire, clinicians should be aware that women, particularly those who are postmenopausal, may not enter the cycle with spontaneous sexual desire, but instead may experience arousal in response to a sexual stimulus followed by desire—ie, responsive rather than spontaneous sexual desire. Sexual arousal may precede desire, especially for women in long-term relationships, and emotional intimacy is a key driver for sexual engagement in women.11