Benefits and pitfalls of open power morcellation of uterine fibroids
The current practice of open power morcellation is being scrutinized by those within and outside of the ObGyn community. We need to re-examine our current use of this procedure.
![]()
Sequelae of open power morcellation
Video courtesy of Javier F. Magrina, MD, Professor, Obstetrics-Gynecology, Mayo Clinic, Phoenix, Arizona; Immediate Past President, AAGL
Vaginal approach to open hand morcellation using a colpotomy incision during hysterectomy
Video courtesy of Javier F. Magrina, MD, Professor, Obstetrics-Gynecology, Mayo Clinic, Phoenix, Arizona; Immediate Past President, AAGL
Vaginal approach to open hand morcellation of a large uterus using a colpotomy incision during hysterectomy
Video courtesy of John B. Gebhart, MD, MS, Associate Professor of Obstetrics and Gynecology, and Fellowship Program Director, Mayo Clinic, Rochester, Minnesota
Morcellation in the News
- Philadelphia hospital restricts 'morcellation' procedure Wall Street Journal, February 20, 2014
- Society of Gynecologic Surgeons releases position statement on morcellation
- Uterine surgical technique is linked to abnormal growths and cancer spread New York Times, February 6, 2014
- Evaluating the risks of electric uterine morcellation JAMA, February 6, 2014. doi:10.1001/jama.2014.1093
- Critics of fibroid removal procedure question risks it may pose for women with undetected uterine cancer JAMA, February 6, 2014. doi:10.001/jama.2014.27
Uterine leiomyomata, also known as fibroids, are the most common pelvic tumor among women. In some women fibroids may be associated with no symptoms. In these cases, the fibroids are often managed expectantly. For many women, however, fibroids cause problems, including heavy uterine bleeding, pelvic pain, and infertility. In these cases removal of the fibroids, either by myomectomy or by hysterectomy, is a common treatment. In the United States, the two most common reasons for performing a hysterectomy are uterine fibroids or abnormal uterine bleeding.1
New minimally invasive gynecologic surgery (MIGS) technology and advanced surgical skills now permit the removal of very large uterine fibroids through small laparoscopic surgery incisions. There are many advantages to MIGS removal of uterine fibroids. The reported benefits include2:
- no large abdominal laparotomy incision
- faster healing and recovery from surgery
- less postoperative pain
- lower risk of surgical site infection
- more rapid return to full activities.
Related Article: Update: Minimally invasive surgery Amy Garcia, MD (April 2012)
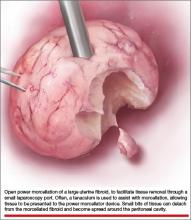
Laparoscopic surgeons often select open power morcellation of the fibroid or fibroid-laden uterus to remove the mass of tissue through a small laparoscopy port. In current MIGS practice, power morcellation typically occurs outside of a closed environment, such as a bag. Open power morcellation of uterine tissue has an important pitfall. This practice permits small bits of tissue to spread around the peritoneal cavity (FIGURE). Given the enhanced growth potential of uterine tumor cells, the postoperative growth of nodules of tissue generated by morcellation is a worrisome possibility.
Morcellation of uterine fibroids and the possibility of causing disseminated leiomyomatosis
Uterine fibroids are clonal tumors that arise from a somatic mutation in a precursor cell. Tumors with clonal somatic mutations have enhanced growth potential because normal mechanisms that control cell growth have been disrupted at the level of cell DNA. Many uterine fibroids demonstrate an abnormal karyotype. Fibroids with a karyotype showing an exchange of genetic material between chromosomes 12 and 14 (t(12;14) (q13-15, q23-24)) are often large.3 The t(12;14) (q13-15, q23-24) translocation is associated with an increased expression of HMGIC, a gene that stimulates cell growth.4
Open morcellation of uterine fibroids may result in the dispersion of bits of tissue around the peritoneal cavity and surgical ports. If the fibroid contains genetic mutations that significantly increase the growth potential of fibroid cells, fibroid nodules may grow postoperatively in the pelvis, abdomen, and surgical ports.5–15 Investigators have called these disseminated nodules of fibroid tumor, “morcellomas.”16
Related Article: Ins and outs of straight-stick laparoscopic myomectomy James Robinson, MD, MS, and Gaby Moawad, MD (September 2012)
Ordulu and colleagues recently reported a case of a woman with uterine fibroids who underwent supracervical hysterectomy using morcellation and 7 years later developed disseminated peritoneal leiomyomatosis (DPL) requiring a second operation.17 Five anatomically distinct DPL masses were karyotyped and showed cytogenetic abnormalities often observed in uterine fibroids with enhanced growth potential, including the t(12;14) (q13-15, q23-24) chromosome translocation. As noted above, the t(12;14) (q13-15, q23-24) translocation is associated with enhanced growth of fibroid tumor cells due, in part, to overexpression of HMGIC.4
Morcellation of occult uterine leiomyosarcomas
In some cases, a uterine tumor thought to be a fibroid is surgically excised, but histologic analysis shows that the tumor is actually a uterine leiomyosarcoma. In surgical case series, approximately 0.08% to 0.13% of uterine masses thought to be due to fibroids are proven by postoperative histology to be a uterine leiomyosarcoma.18–20 Most leiomyosarcomas are Stage I,21 but if the sarcoma tissue is open power morcellated in the peritoneal cavity, bits of tissue can be spread, upstaging the tumor and worsening the prognosis.22
In one retrospective study of women with leiomyosarcoma, the 5-year estimated survival was 73% if the tumor was removed without morcellation and 46% if the tumor was removed using morcellation.22 If a “fibroid” or “fibroid uterus” is power morcellated, but the final histology reveals leiomyosarcoma, surgical re-exploration will be recommended to detect any spread of cancer, and chemotherapy may be necessary if tumor spread is detected.23,24
Many experts recommend a standardized preoperative evaluation of all cases of presumed uterine fibroid tumors where open power morcellation of tissue is planned. Recommended preoperative studies include25: