ObGyns’ choice of practice environment is a big deal
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
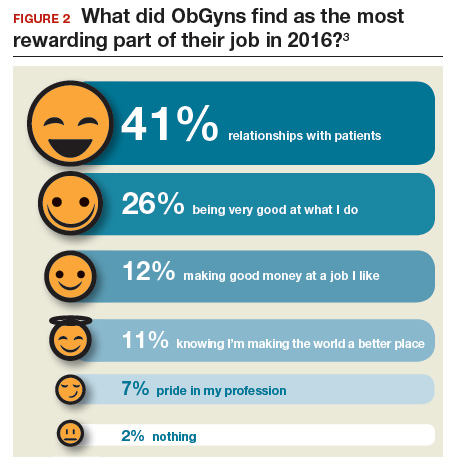
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
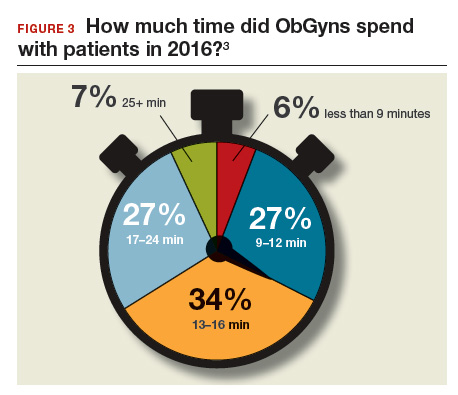
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations






