Surgical strategies to untangle a frozen pelvis
Few surgeries require the judgment, rigorous experience, and skill necessary to operate on a frozen pelvis
IN THIS ARTICLE
Handle the ureter gently
Never handle the ureter excessively or unnecessarily. When it is dissected free, let it lie free rather than retracting it with umbilical tapes or Penrose drains, which can slide up and down, damaging the vasculature that lies in the adventitia of the ureteral wall.
A history of surgery in the area of the bladder, such as cesarean section or bladder advancement with uterine suspension, may leave the bladder adherent to or hard to separate from the cervix and vagina. Normally, the vesicouterine peritoneum is flexible, mobile, and easy to free from the cervix and vagina. A history of disease processes such as endometriosis, infection, or tumors makes this dissection difficult, with a real risk of inadvertent cystotomy.
One technique to make this dissection easier and safer is to enter the retroperitoneum laterally near the round ligament. In this location, the bladder may not have been involved in the prior dissection, and the tissue may be more areolar and less dense than it is in the midline. After entering the retroperitoneum, elevate the bladder by incising the vesicouterine peritoneum transversely. By rolling a finger or an instrument cephalad in the anterior leaf of the broad ligament, the bladder can be sharply separated from the cervix.
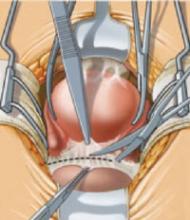
When the bladder is densely adherent, make an incision into its dome away from the cervix to visualize the interior of the bladder. Place the index finger into the bladder to identify its reflection, and cut through the dense adhesions between it and the cervix and vagina (FIGURE 3).
FIGURE 3 Incise the broad-ligament peritoneum
Incise the peritoneum of the avascular layer of the anterior broad ligament bilaterally between the divided round ligaments to develop the vesical space bilaterally. One way to do this is to gently tease away the areolar tissue using a finger, pushing the tissue medially. Then divide the peritoneum between the 2 spaces and sweep the bladder off the cervix using blunt or sharp dissection.
Cul-de-sac of Douglas may be hard to recognize
In a disease-free pelvis, the posterior cul-de-sac is bounded laterally by the uterosacral ligaments, posteriorly by the rectum and sacrum, and caudally by the vagina—but these relationships are usually lost in the frozen pelvis. Extensive inflammatory disease, tumors of the tubes and ovaries, extensive pelvic endometriosis, and prior infection due to a diverticular abscess or ruptured appendix can obscure the normal confines of the cul-de-sac. It can also be obliterated by large myomas, which can fill the pelvic cavity and extend upward beyond the sacral promontory into the abdominal cavity, thereby displacing the intestines and creating potential deviation and compression of the ureters.
Freeing the peritoneal attachments both anteriorly and posteriorly, as well as at the sides of the pelvis, may release the pelvic contents and allow elevation of the uterus into the abdominal cavity. Then the ureter, uterine vasculature, and supporting ligaments can be identified. Dissection becomes simpler after this point.
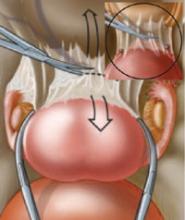
However, when the rectum and ureters are densely adherent, as they often are in the frozen pelvis, dissection can become difficult, with a real danger of rectal perforation. A basic principle in any hysterectomy is to hug the uterus as closely as possible, staying near the posterior surface of the uterus and cervix using both blunt and sharp dissection. This eventually makes it possible to find a reasonable plane to enter the rectovaginal space at the superior portion of the cul-de-sac between the uterosacral ligaments.
The tissue below this level is not usually involved in the frozen pelvis and will give way readily once the uterosacral ligaments are divided. It is unnecessary to operate beyond this level to any great extent because the surgery already extends distal to the cervicovaginal junction. In some circumstances, it may be necessary to enter the vagina anteriorly to define the relationship between the posterior cervix and adherent bowel (FIGURE 4).
FIGURE 4 Mobilize the uterus
To free the uterus from its posterior visceral attachments and render it mobile, develop the rectovaginal space.
Identifying and repairing bowel injury
If the bowel has been prepped, and rectal enterotomy occurs during dissection, closure and drainage are the only necessary steps, and a temporary colostomy can be avoided. Bowel resection may be necessary if the bowel has sustained damage.
If bowel injury is suspected, irrigate the bowel through the rectum with sterile milk or dye solution using a Foley catheter with a 30-cc bag. Another widely used option to assess rectosigmoid integrity is to insufflate the submersed rectosigmoid with air. Bubbles signal a breach in the integrity of the bowel wall.