Gynecologic care of the cancer patient
As more Ob/Gyns provide follow-up care to patients who have survived cancer, there is an increased need for information on how to better care for these women with regard to menopause, risk for subsequent disease, and preventive care.
It is beyond the scope of this article to delineate or evaluate the many herbal and nutritional supplements available for the management of vasomotor symptoms. According to the literature, their efficacy is questionable. Nonetheless, the industries that promote these products are among the fastest-growing businesses, largely due to the public’s fears about breast cancer.
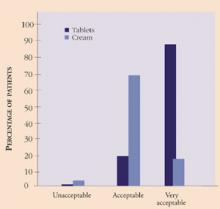
Genitourinary symptoms. Atrophic changes of the vagina are common in the menopausal years and are associated with generalized pruritus and dyspareunia to variable degrees in each individual. This, in addition to the cancer diagnosis and treatment, can lead to symptoms of depression, low self-esteem, and relationship issues surrounding sexuality. It is essential to address symptoms of vaginal atrophy and discuss treatment options with the cancer patient. Local estrogen therapy in the form of a 17-beta estradiol-releasing ring or tablet is an effective method22,23 and has been used successfully in breast cancer survivors at our institution. Since the absorption of estrogen is minimal, it is thought to be safe.24 Further, the risk of endometrial cancer associated with the use of unopposed estrogen is lower with the vaginal ring or tablet than with estrogen cream, as evidenced by endometrial biopsies (TABLE 1).22 In addition, it appears patient satisfaction and acceptability, i.e., ease and comfort of administration, is greater with the tablet than with the cream (Figure 1).
FIGURE 1 Patient satisfaction with vaginal tablets and cream
Source: Rioux JE, Devlin C, Gelfrand M, et al. 17-beta estradiol vaginal tablet versus conjugated equine estrogen cream to relieve menopausal atrophic vaginitis. Menopause. 2000;7:156-161.TABLE 1
Safety of vaginal tablets versus cream for the treatment of atrophic vaginitis
| VAGINAL TABLETS (N=80) | VAGINAL CREAM (N=79) | |||
|---|---|---|---|---|
| BASELINE | WEEK 34 | BASELINE | WEEK 24 | |
| Patients with biopsies/stained biopsies | 60 | 49 | 59 | 49 |
| Atrophic endometrium | 34 | 34 | 35 | 15 |
| Weakly proliferative endometrium | 1 | 0 | 3 | 4 |
| Proliferative endometrium | 0 | 1 | 1 | 7 |
| Endometrial hyperplasia | 0 | 0 | 0 | 2 |
| Biopsies with insufficient tissue | 25 | 14 | 20 | 21 |
| Source: Rioux JE, Devlin C, Gelfrand M, et al. 17-beta estradiol vaginal tablet versus conjugated equine estrogen cream to relieve menopausal atrophic vaginitis. Menopause. 2000;7:156-161. | ||||
Screening for genetic mutations
Genetic counseling should be offered to all patients who appear to carry an increased cancer risk based on their personal or family histories. Unfortunately, many women with a history of breast or ovarian cancer have never been offered such counseling. Therefore, it is important for Ob/Gyns to screen cancer survivors to identify those patients at risk for subsequent disease.
Although most cancers arise from somatic mutations acquired after birth, approximately 10% of both breast and ovarian cancers are thought to result from inherited gene mutations that are passed down through the maternal or paternal lines. The theory that some breast and ovarian cancers have a genetic basis has been entertained for decades, but only recently have the gene mutations BRCA1 and BRCA2 been identified.25,26 Approximately 85% of hereditary breast carcinomas result from alterations in the BRCA1 and BRCA2 genes.27 These genes also are responsible for most inherited ovarian carcinomas.
Studies also have shown that in families with a history of ovarian cancer or early-onset breast cancer, the risk of developing breast cancer by age 70 is more than 80% for women with BRCA1 or BRCA2 mutations.26,28-30 The risk of developing breast cancer before the age of 50 is 33% to 50% in women with a gene mutation in BRCA1 or BRCA2, versus only 2% in a woman without a gene mutation.30,31
The risk of ovarian cancer conferred by mutations in BRCA1 appears to be greater than that for BRCA2. The BRCA1 mutation is associated with a risk of ovarian cancer between 28% and 44% by age 70, as compared to 1.8% in the general population.28,30,32 The BRCA2-associated risk of ovarian cancer is estimated at 27%, with most cases occurring after the age of 50. TABLE 2 summarizes the risk of cancer conferred by inherited mutations in BRCA1 and BRCA2.
Three forms of hereditary epithelial ovarian cancer exist.26,28,33,34 The most common form appears as a component of the hereditary breast/ovarian cancer syndrome. In these families, multiple cases of breast and ovarian cancer are found, and mutations in the BRCA1 gene are thought to account for the vast majority of them.
The second form of hereditary ovarian cancer occurs as site-specific cancer and is inherited as an autosomal-dominant trait. Mutations in BRCA1 also account for a large proportion of these cases. The third form of hereditary ovarian cancer occurs as a component of the hereditary nonpolyposis colorectal cancer (HNPCC) syndrome. It is characterized by an autosomal-dominant transmission of nonpolyposis colon cancer along with adenocarcinomas of the ovary, uterus, breast, kidney, stomach, pancreas, small bowel, and biliary tree.35
The hallmark of hereditary ovarian cancers is their occurrence at a younger age, the mean being in the mid-40s, with 17% occurring by age 40.36 Therefore, if prophylactic surgery is considered, it generally should be performed prior to the end of the fourth decade of life, after the patient has completed child-bearing. However, since some cases of hereditary ovarian cancer occur in later life, it is thought that even a woman in her 60s or 70s may benefit from prophylactic surgery. Patients undergoing the surgery should be counseled that while their risk is reduced significantly, it is not eliminated. Primary peritoneal carcinomatosis remains a possibility; this risk is estimated at 2% to 11% for women who have undergone prophylactic surgery.37,38