Improving Hand Hygiene Adherence in Healthcare Workers Before Patient Contact: A Multimodal Intervention in Four Tertiary Care Hospitals in Japan
OBJECTIVES: Our objectives were to evaluate hand hygiene adherence among physicians and nurses before touching hospitalized patients and to evaluate changes in hand hygiene adherence after a multimodal intervention was implemented.
DESIGN, SETTING, AND PARTICIPANTS: We conducted a pre- and postintervention study with HCWs at four tertiary hospitals in Niigata, Japan. Hand hygiene observations were conducted from June to August 2018 (preintervention) and February to March 2019 (postintervention).
INTERVENTION: The multimodal hand hygiene intervention recommended by the World Health Organization was tailored to each hospital and implemented from September 2018 to February 2019.
MAIN OUTCOMES AND MEASURES: We observed hand hygiene adherence before touching patients in each hospital and compared rates before and after intervention. Intervention components were also evaluated.
RESULTS: There were 2,018 patient observations preintervention and 1,630 postintervention. Overall, hand hygiene adherence improved from 453 of 2,018 preintervention observations (22.4%) to 548 of 1,630 postintervention observations (33.6%; P < .001). Rates improved more among nurses (13.9 percentage points) than among doctors (5.7 percentage points). Improvement varied among the hospitals: Hospital B (18.4 percentage points) was highest, followed by Hospitals D (11.4 percentage points), C (11.3 percentage points), and Hospital A (6.5 percentage points).
CONCLUSIONS: A multimodal intervention improved hand hygiene adherence rates in physicians and nurses in Niigata, Japan; however, further improvement is necessary. Given the current suboptimal hand hygiene adherence rates in Japanese hospitals, the spread of COVID-19 within the hospital setting is a concern.
© 2020 Society of Hospital Medicine
METHODS
Participating hospitals
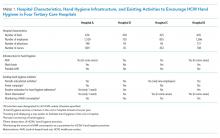
Four tertiary care hospitals in Niigata, Japan, volunteered to participate in the study. The characteristics of the four participating hospitals are summarized in Table 1. All hospitals are public or community based. Hospital A included two units, consisting of a cardiovascular-cerebral ICU and an emergency department (ED), and Hospitals B, C, and D included various units containing surgical or medical wards, an ICU, or an ED. All four hospitals have at least one designated infection-prevention nurse and an infection-prevention department. In addition, there is an infection control network system among the hospitals, and they communicate well to update the information related to local, domestic, or global infectious diseases through regular seminars and by distributing and exchanging electronic communication.
Preintervention
The preintervention infrastructure and existing activities to improve HCW hand hygiene in each hospital are summarized in Table 1. These activities were developed by each individual hospital and had been in place for at least 6 months before the study intervention. All hospitals used AHR and did direct observation for hand washing in designated wards or units and monitoring of AHR consumption; however, Hospital B did not have a wash basin in each room and no use of portable AHR. Preintervention hand hygiene data were collected from June to August 2018.
Intervention
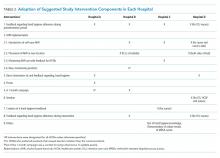
To improve hand hygiene adherence, we initiated a multimodal intervention from September 2018 to February 2019 based on WHO recommendations13 and the findings from prior hand hygiene studies.22 Each facility was provided the same guidance on how to improve hand hygiene adherence and was asked to tailor their intervention to their settings (Table 2 and Appendix Figure). Suggested interventions included feedback regarding hand hygiene adherence observed during the preintervention period, interventions related to AHR, direct observation of and feedback regarding hand hygiene, new posters promoting hand hygiene in the workplace, a 1-month campaign for hand hygiene, seminars for HCWs related to hand hygiene, creation of a handbook for education/training, feedback regarding hand hygiene adherence during the intervention period, and others. The infection control team at each hospital designed the plans and strategies to improve hand hygiene adherence. Postintervention data were collected from February 2019 to March 2019.
Observation of Hand Hygiene Adherence
Hand hygiene adherence before patient contact was evaluated by board-certified infection control nurses. To reduce observation bias, external nurses from other participating hospitals conducted the observations. To minimize intraobserver variation, the same training as the previous study in Japan21 was provided. Hand hygiene observations were usually performed during the day Monday to Friday from 8
Use of either AHR or soap and water before patient contact was defined as appropriate hand hygiene.24,25 Hand hygiene adherence before patient contact for each provider-patient encounter was observed and recorded using a data collection form used in the previous studies.19,26 The following information was obtained: unit name, time of initiation and completion of observations, HCW type (physician or nurse), and the type of hand hygiene (ie, AHR, hand washing with soap and water, or none). The observers kept an appropriate distance from the observed HCWs to avoid interfering with their regular clinical practice. In addition, we informed HCWs in the hospital that their clinical practices were going to be observed; however, they were not informed their hand hygiene adherence was going to be monitored.