Portable Ultrasound Device Usage and Learning Outcomes Among Internal Medicine Trainees: A Parallel-Group Randomized Trial
BACKGROUND: Little is known about how to effectively train residents with point-of-care ultrasonography (POCUS) despite increasing usage.
OBJECTIVE: This study aimed to assess whether handheld ultrasound devices (HUDs), alongside a year-long lecture series, improved trainee image interpretation skills with POCUS.
METHODS: Internal medicine intern physicians (N = 149) at a single academic institution from 2016 to 2018 participated in the study. The 2017 interns (n = 47) were randomized 1:1 to receive personal HUDs (n = 24) for patient care vs no-HUDs (n = 23). All 2017 interns received a repeated lecture series regarding cardiac, thoracic, and abdominal POCUS. Interns were assessed on their ability to interpret POCUS images of normal/abnormal findings. The primary outcome was the difference in end-of-the-year assessment scores between interns randomized to receive HUDs vs not. Secondary outcomes included trainee scores after repeating lectures and confidence with POCUS. Intern scores were also compared with historical (2016, N = 50) and contemporaneous (2018, N = 52) controls who received no lectures.
RESULTS: Interns randomized to HUDs did not have significantly higher image interpretation scores (median HUD score: 0.84 vs no-HUD score: 0.84; P = .86). However, HUD interns felt more confident in their abilities. The 2017 cohort had higher scores (median 0.84), compared with the 2016 historical control (median 0.71; P = .001) and 2018 contemporaneous control (median 0.48; P < .001). Assessment scores improved after first-time exposure to the lecture series, while repeated lectures did not improve scores.
CONCLUSIONS: Despite feeling more confident, personalized HUDs did not improve interns’ POCUS-related knowledge or interpretive ability. Repeated lecture exposure without further opportunities for deliberate practice may not be beneficial for mastering POCUS.
© 2020 Society of Hospital Medicine
Surveys
Surveys were administered alongside the assessments to the 2016-2018 intern classes. These surveys assessed trainee attitudes toward POCUS and were based on previously validated assessments.27,28,30 Attitudes were measured using 5-point Likert scales.
Statistical Analysis
For the primary outcome, we performed generalized binomial mixed-effect regressions using the survey periods, randomization group, and the interaction of the two as independent variables after adjusting for attendance and controlling of intra-intern correlations. The bivariate unadjusted analysis was performed to display the distribution of overall correctness on the assessments. Wilcoxon signed rank test was used to determine score significance for dependent score variables (R-Statistical Programming Language, Vienna, Austria).
RESULTS
Baseline Characteristics
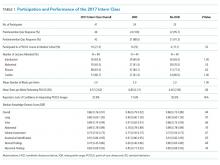
There were 149 interns who participated in this study (Figure). Assessment/survey completion rates were as follows: 2016 control: 68.0%; 2017 preintervention: 97.9%; 2017 postintervention: 89.4%; and 2018 control: 100%. The 2017 interns reported similar amounts of prior POCUS exposure in medical school (Table 1).
Primary Outcome: Assessment Scores (HUD vs no HUD)
There were no significant differences in assessment scores at the end of the study between interns randomized to personal HUD access vs those to no-HUD access (Table 1). HUD interns reported performing POCUS assessments on patients a mean 6.8 (standard deviation [SD] 2.2) times per week vs 6.4 (SD 2.9) times per week in the no-HUD arm (P = .66). The mean lecture attendance was 75.0% and did not significantly differ between the HUD arms (Table 1).
Secondary Outcomes
Impact of Repeating Lectures
The 2017 interns demonstrated significant increases in preblock vs postblock assessment scores after first-time exposure to the lectures (median preblock score 0.61 [interquartile range (IQR), 0.53-0.70] vs postblock score 0.81 [IQR, 0.72-0.86]; P < .001; Table 2). However, intern performance on the preblock vs postblock assessments after second-time exposure to the curriculum failed to improve (median second preblock score 0.78 [IQR, 0.69-0.83] vs postblock score 0.81 [IQR, 0.64-0.89]; P = .94). Intern performance on individual domains of knowledge for each block is listed in Appendix Table 1.
Intervention Performance vs Controls
The 2016 historical control had significantly higher scores compared with the 2017 preintervention group (P < .001; Appendix Table 2). The year-long lecture series resulted in significant increases in median scores for the 2017 group (median preintervention score 0.55 [0.41-0.61] vs median postintervention score 0.84 [0.71-0.90]; P = .006; Appendix Table 1). At the end of the study, the 2017 postintervention scores were significantly higher across multiple knowledge domains compared with the 2016 historical control (Appendix Table 2).
Survey Results
Notably, the 2017 intern class at the end of the intervention did not have significantly different assessment scores for several disease-specific domains, compared with the 2016 control (Appendix Table 2). Nonetheless, the 2017 intern class reported higher levels of confidence in these same domains despite similar scores (Supplementary Figure). The HUD group seldomly cited a lack of confidence in their abilities as a barrier to performing POCUS examinations (17.6%), compared with the no-HUD group (50.0%), despite nearly identical assessment scores between the two groups (Table 1).