The Association between Limited English Proficiency and Sepsis Mortality
BACKGROUND: Limited English proficiency (LEP) has been implicated in poor health outcomes. Sepsis is a frequently fatal syndrome that is commonly encountered in hospital medicine. The impact of LEP on sepsis mortality is not currently known.
OBJECTIVE: To determine the association between LEP and sepsis mortality. DESIGN: Retrospective cohort study.
SETTING: 800-bed, tertiary care, academic medical center.
PATIENTS: Electronic health record data were obtained for adults admitted to the hospital with sepsis between June 1, 2012 and December 31, 2016.
MEASUREMENTS: The primary predictor was LEP. Patients were defined as having LEP if their self-reported primary language was anything other than English and interpreter services were required during hospitalization. The primary outcome was inpatient mortality. Mortality was compared across races stratified by LEP using chi-squared tests of significance. Bivariable and multivariable logistic regressions were performed to investigate the association between mortality, race, and LEP, adjusting for baseline characteristics, comorbidities, and illness severity.
RESULTS: Among 8,974 patients with sepsis, we found that 1 in 5 had LEP, 62% of whom were Asian. LEP was highly associated with death across all races except those identifying as Black and Latino. LEP was associated with a 31% increased odds of mortality after adjusting for illness severity, comorbidities, and other baseline characteristics, including race (OR 1.31, 95% CI 1.06-1.63, P = .02).
CONCLUSIONS: In a single-center study of patients hospitalized with sepsis, LEP was associated with mortality across nearly all races. This is a novel finding that will require further exploration into the causal nature of this association.
© 2019 Society of Hospital Medicine
RESULTS
We identified 8,974 patients hospitalized with sepsis based on the above inclusion criteria. This represented a medically complex, racially and linguistically diverse population (Table 1). The cohort was comprised of 24% Asian, 12% Black, and 11% Latino patients. Among those categorized as Other race, Native Americans/Alaskan Natives and Native Hawaiians/Pacific Islanders accounted for 4% (n = 31) and 21% (n = 159), respectively. A fifth of all patients had LEP (n = 1,716), 62% of whom were Asian (n = 1,064). Patients with LEP tended to be older, female, and to have a greater number of comorbid conditions (Table 1). The total qualifying SOFA score was also higher among patients with LEP (median 5; interquartile range [IQR]: 4-8 vs 5; IQR: 3-7; P <.001), though there was no association between LEP and mechanical ventilation (P = .22). The prevalence of LEP differed significantly across races, with 50% LEP among Asians, 32% among Latinos, 5% among White patients (P < .001). Only eight Black patients had LEP. More than 40 unique languages were represented in the cohort, with English, Cantonese, Spanish, Russian, and Mandarin accounting for ~95% (Appendix Table 1). Among Latino patients, 63% spoke English and 36% spoke Spanish.
In-hospital mortality was significantly higher among patients who had LEP (n = 268/1,716, 16%) compared to non-LEP patients (n = 678/7,258, 9%), with 80% greater unadjusted odds of mortality (OR 1.80; 95% CI: 1.54-2.09; P < .001). Notably we also found that Asian race was associated with a 1.57 unadjusted odds of mortality compared to White race (95% CI: 1.34-1.85; P < .001). Age, VWS, total qualifying SOFA score, mechanical ventilation, and admission level of care all exhibited a positive dose-response association with mortality (Appendix Table 2). In unadjusted analyses, there was no evidence of interaction between LEP and age (P = .38), LEP and race (P = .45), LEP and ICU admission level of care (P = .31), or LEP and mechanical ventilation (P = .19). Asian patients had the highest overall mortality (14% total, 17% with LEP). LEP was associated with increased unadjusted mortality among White, Asian, and Other races compared to their non-LEP counterparts (Appendix Figure 1). There was no significant difference in mortality between Latino patients with and without LEP. The sample size for Black patients with LEP (n = 8) was too small to draw conclusions about mortality.
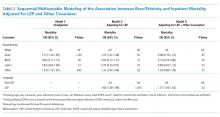
Following multivariable logistic regression modeling for the association between race and mortality, we found that the increased odds of death among Asian patients was partially attenuated after adjusting for LEP (odds ratio [OR] 1.23, 95% CI: 1.02-1.48; P = .03; Table 2). Meanwhile, LEP was associated with a 1.66 odds of mortality (95% CI: 1.38-1.99; P < .001) after adjustment for race. In the full multivariable model adjusting for demographics and clinical characteristics, illness severity, and comorbidities, LEP was associated with a 31% increase in the odds of mortality compared to non-LEP (95% CI: 1.06-1.63; P = .02). In this model, the association between Asian race and mortality was now fully attenuated, with a point estimate near 1.0 (OR 0.98; 95% CI: 0.79-1.22; P = .87). Markers of illness severity, including total qualifying SOFA score (OR 1.23; 95% CI: 1.20-1.27; P < .001) and need for mechanical ventilation (OR 1.88; 95% CI: 1.52-2.33; P < .001), were both associated with greater odds of death. Based on a four-step mediation analysis, LEP was found to be a partial mediator to the association between Asian race and mortality (76% proportion explained). The E-value for the association between LEP and mortality was 1.95, with an E-value for the corresponding confidence interval of 1.29.
In a subgroup analysis using the fully adjusted model restricted to patients who were mechanically ventilated during hospitalization, the association between LEP and mortality was no longer present (OR 1.15; 95% CI: 0.76-1.72; P = .51).