Antibiotics for Aspiration Pneumonia in Neurologically Impaired Children
OBJECTIVE: To compare hospital outcomes associated with commonly used antibiotic therapies for aspiration pneumonia in children with neurologic impairment (NI).
DESIGN/METHODS: A retrospective study of children with NI hospitalized with aspiration pneumonia at 39 children’s hospitals in the Pediatric Health Information System database. Exposure was empiric antibiotic therapy classified by antimicrobial activity. Outcomes included acute respiratory failure, intensive care unit (ICU) transfer, and hospital length of stay (LOS). Multivariable regression evaluated associations between exposure and outcomes and adjusted for confounders, including medical complexity and acute illness severity.
RESULTS: In the adjusted analysis, children receiving Gram-negative coverage alone had two-fold greater odds of respiratory failure (odds ratio [OR] 2.15; 95% CI: 1.41-3.27), greater odds of ICU transfer (OR 1.80; 95% CI: 1.03-3.14), and longer LOS [adjusted rate ratio (RR) 1.28; 95% CI: 1.16-1.41] than those receiving anaerobic coverage alone. Children receiving anaerobic and Gram-negative coverage had higher odds of respiratory failure (OR 1.65; 95% CI: 1.19-2.28) than those receiving anaerobic coverage alone, but ICU transfer (OR 1.15; 95% CI: 0.73-1.80) and length of stay (RR 1.07; 95% CI: 0.98-1.16) did not statistically differ. For children receiving anaerobic, Gram-negative, and P. aeruginosa coverage, LOS was shorter (RR 0.83; 95% CI: 0.76-0.90) than those receiving anaerobic coverage alone; odds of respiratory failure and ICU transfer rates did not significantly differ.
CONCLUSIONS: Anaerobic therapy appears to be important in the treatment of aspiration pneumonia in children with NI. While Gram-negative coverage alone was associated with worse outcomes, its addition to anaerobic therapy may not yield improved outcomes.
© 2019 Society of Hospital Medicine
Generalized linear mixed-effects models with random hospital intercepts were derived to assess the independent effect of antimicrobial spectra of activity on outcomes of acute respiratory failure, ICU transfer, and LOS while adjusting for important differences in demographic and clinical characteristics. LOS had a nonnormal distribution. Thus, we used an exponential distribution. Covariates were chosen a priori given the clinical and biological relevance to exposure and outcomes—age, presence of complex chronic condition diagnoses, the number of complex chronic conditions, technology dependence, the performance of diagnostic tests on presentation, and illness severity on presentation. ICU admission was included as a covariate in acute respiratory failure and LOS outcome models. The results of the model for acute respiratory failure and ICU transfer are presented as adjusted odds ratios (OR) with a 95% CI. LOS results are presented as adjusted rate ratios (RR) with 95% CI.
All analyses were performed with SAS 9.3 (SAS Institute, Cary, North Carolina). P values <.05 were considered statistically significant. Cincinnati Children’s Hospital Medical Center Institutional Review Board considered this deidentified dataset study as not human subjects research.
RESULTS
Study Cohort
At the 44 hospitals included, 4,812 children with NI hospitalized with the diagnosis of aspiration pneumonia met the eligibility criteria. However, 79 received antibiotics with the spectra of activity not examined, leaving 4,733 children in our final analysis (Appendix Figure). Demographic and clinical characteristics of the study cohort are shown in Table 1. Median age was five years (interquartile range [IQR]: 2-11 years). Most subjects were male (53.9%), non-Hispanic white (47.9%), and publicly insured (63.6%). There was a slight variation in the distribution of admissions across seasons (spring 31.6%, summer 19.2%, fall 21.3%, and winter 27.9%). One-third of children had four or more comorbid CCCs (complex chronic conditions; 34.2%). The three most common nonneurologic CCC diagnosis categories were gastrointestinal (63.1%), congenital and/or genetic defects (36.9%), and respiratory (8.9%). Assistance with medical technologies was also common (82%)—particularly gastrointestinal (63.1%) and neurologic/neuromuscular (9.8%) technologies. The vast majority of children (92.5%) had either a chest radiograph (90.5%), respiratory viral study (33.7%), or respiratory culture (10.0%) obtained on presentation. A minority required noninvasive or invasive respiratory support (25.4%), vasoactive agents (8.9%), blood products (1.2%), or pleural drainage (0.3%) in the first two hospital days.
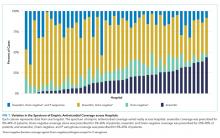
Spectrum of Antimicrobial Coverage
Most children (57.9%) received anaerobic and Gram-negative coverage; 16.2% received anaerobic, Gram-negative and P. aeruginosa coverage; 15.3% received anaerobic coverage alone; and 10.6% received Gram-negative coverage alone. Empiric antimicrobial coverage varied substantially across hospitals: anaerobic coverage was prescribed for 0%-44% of patients; Gram-negative coverage was prescribed for 3%-26% of patients; anaerobic and Gram-negative coverage was prescribed for 25%-90% of patients; and anaerobic, Gram-negative, and P. aeruginosa coverage was prescribed for 0%-65% of patients (Figure 1).