The American Board of Pediatrics Response to the Pediatric Hospital Medicine Petition
© 2019 Society of Hospital Medicine
PRACTICE PATHWAY CRITERIA USED IN THE APPLICATION PROCESS
PHM is the 15th pediatric subspecialty to begin the certification process with a practice pathway. In none of the prior cases was it possible to do a detailed implementation study to understand the myriad of ways in which individual pediatricians arrange their professional and personal time. This reality has led to the publication of only general, rather than specific practice pathway criteria at the start of the application process for PHM and every other pediatric subspecialty. Rather, in each case, a well-informed and diverse peer group of subspecialists (the subboard) has reviewed the applications to get a sense of the variations of practice and then decided on the criteria that a subspecialist must meet to be considered eligible to sit for the certifying exam. Clear-cut criteria were used consistently in adjudicating all applications. Although the ABP has not done this for other subspecialties, we agree that publishing the specific criteria once they had been decided upon would have improved the process. We commit to doing so in the future.
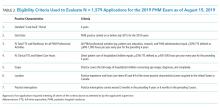
The eligibility criteria were designed to be true to the mission of the ABP and seek parity with the requirements used by other subspecialties and by the PHM training pathway. The assumption is that competent PHM practice of sufficient duration and breadth, attested to by a supervisor, would allow the ABP to represent to the public that the candidate is qualified to sit for the exam. The eligibility criteria focused on seven practice characteristics (Table 2):
(2) The July 2015 start date follows from the four-year look-back window for the November 2019 exam date.
(3) The minimum percentage full-time equivalent (%FTE) for all PHM professional activities (ie, clinical care, research, education, and PHM administration) was set at 50% FTE. Recognizing that an FTE may be defined differently at different institutions, the ABP defined the workweek as 40 hours and the 50% FTE as 900-1,000 hours per year.
(4) The minimum percentage FTE for PHM direct patient care (as described below) was set at 25% FTE and defined as 450-500 hours per year. Every candidate must satisfy both the minimum hours for all PHM professional activities and the minimum hours for the direct care of hospitalized children. Applicants must meet or exceed these minima if the ABP is to represent to the public that an applicant has the necessary experience to be called a subspecialist. Similarly, all other ABP subspecialties required at least 50% FTE commitment for the candidate to be considered a subspecialist.
(5) The scope of practice seeks to maintain parity with the training pathway by requiring care of the full spectrum of hospitalized children. This full spectrum is defined as children on general pediatric wards, ages birth to 21 years, and specifically includes children with complex chronic disease, surgical care and comanagement, sedation, palliative care, and common procedures. Care devoted exclusively to a narrow patient population (“niched care”), such as newborns in the nursery, does not meet the eligibility requirements.
(6) The location for patient care must have occurred in the United States or Canada.
(7) The possibility of practice interruption was included among the eligibility criteria. Attempting to strike a balance between an applicant demonstrating sufficient recent experience to be called a subspecialist versus the reality of some individuals needing to interrupt professional and clinical practice, the subboard stipulated that interruptions of PHM professional activities should not exceed three months during the preceding four years and six months during the preceding five years.