Cognitive Biases Influence Decision-Making Regarding Postacute Care in a Skilled Nursing Facility
BACKGROUND: Decisions about postacute care are increasingly important as the United States population ages, its use becomes increasingly common, and payment reforms target postacute care. However, little is known about how to improve these decisions.
OBJECTIVE: To understand whether cognitive biases play an important role in patient and clinician decision-making regarding postacute care in skilled nursing facilities (SNFs) and identify the most impactful biases.
DESIGN: Secondary analysis of 105 semistructured interviews with patients, caregivers, and clinicians.
SETTING: Three hospitals and three SNFs in a single metropolitan area.
PATIENTS: Adults over age 65 discharged to SNFs after hospitalization as well as patients, caregivers, and multidisciplinary frontline clinicians in both hospital and SNF settings.
MEASUREMENTS: We identified potential cognitive biases from prior systematic and narrative reviews and conducted a team-based framework analysis of interview transcripts to identify potential biases.
RESULTS: Authority bias/halo effect and framing bias were the most prevalent and seemed the most impactful, while default/status quo bias and anchoring bias were also present in decision-making about SNFs.
CONCLUSIONS: Cognitive biases play an important role in decision-making about postacute care in SNFs. The combination of authority bias/halo effect and framing bias may synergistically increase the likelihood of patients accepting SNFs for postacute care. As postacute care undergoes a transformation spurred by payment reforms, it is increasingly important to ensure that patients understand their choices at hospital discharge and can make high-quality decisions consistent with their goals.
© 2020 Society of Hospital Medicine
METHODS
Study Design
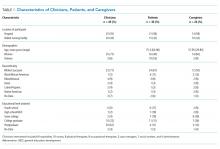
We conducted a secondary analysis on interviews with hospital and SNF clinicians as well as patients and their caregivers who were either leaving the hospital for an SNF or newly arrived in an SNF from the hospital to understand if cognitive biases were present and how they manifested themselves in a real-world clinical context.19 These interviews were part of a larger qualitative study that sought to understand how clinicians, patients, and their caregivers made decisions about postacute care, particularly related to SNFs.13,14 This study represents the analysis of all our interviews, specifically examining decision-making bias. Participating sites, clinical roles, and both patient and caregiver characteristics (Table 1) in our cohort have been previously described.13,14
Analysis
We used a team-based approach to framework analysis, which has been used in other decision-making studies14, including those measuring cognitive bias.20 A limitation in cognitive bias research is the lack of a standardized list or categorization of cognitive biases. We reviewed prior systematic17,21 and narrative reviews18,22, as well as prior studies describing examples of cognitive biases playing a role in decision-making about therapy20 to construct a list of possible cognitive biases to evaluate and narrow these a priori to potential biases relevant to the decision about postacute care based on our prior work (Table 2).
We applied this framework to analyze transcripts through an iterative process of deductive coding and reviewing across four reviewers (ML, RA, AL, CL) and a hospitalist physician with expertise leading qualitative studies (REB).
Intercoder consensus was built through team discussion by resolving points of disagreement.23 Consistency of coding was regularly checked by having more than one investigator code individual manuscripts and comparing coding, and discrepancies were resolved through team discussion. We triangulated the data (shared our preliminary results) using a larger study team, including an expert in behavioral economics (SRG), physicians at study sites (EC, RA), and an anthropologist with expertise in qualitative methods (CL). We did this to ensure credibility (to what extent the findings are credible or believable) and confirmability of findings (ensuring the findings are based on participant narratives rather than researcher biases).
RESULTS
We reviewed a total of 105 interviews with 25 hospital clinicians, 20 SNF clinicians, 21 patients and 14 caregivers in the hospital, and 15 patients and 10 caregivers in the SNF setting (Table 1). We found authority bias/halo effect; default/status quo bias, anchoring bias, and framing was commonly present in decision-making about postacute care in a SNF, whereas there were few if any examples of ambiguity aversion, availability heuristic, confirmation bias, optimism bias, or false consensus effect (Table 2).
Authority Bias/Halo Effect
While most patients deferred to their inpatient teams when it came to decision-making, this effect seemed to differ across VA and non-VA settings. Veterans expressed a higher degree of potential authority bias regarding the VA as an institution, whereas older adults in non-VA settings saw physicians as the authority figure making decisions in their best interests.
Veterans expressed confidence in the VA regarding both whether to go to a SNF and where to go: